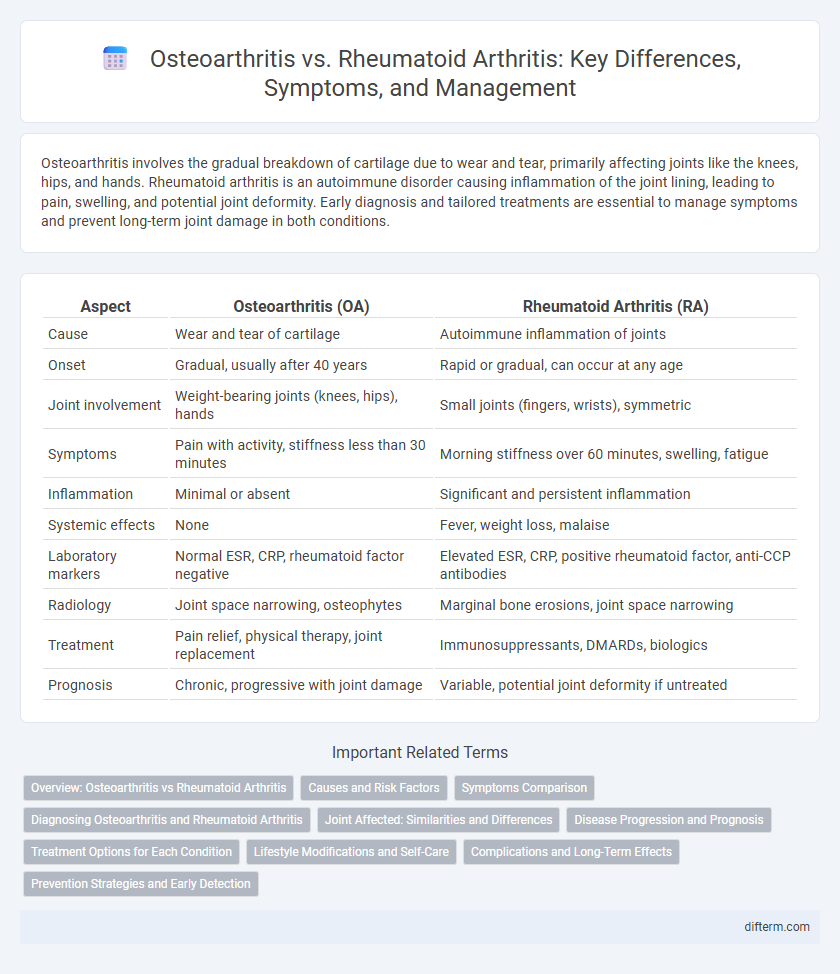
Osteoarthritis involves the gradual breakdown of cartilage due to wear and tear, primarily affecting joints like the knees, hips, and hands. Rheumatoid arthritis is an autoimmune disorder causing inflammation of the joint lining, leading to pain, swelling, and potential joint deformity. Early diagnosis and tailored treatments are essential to manage symptoms and prevent long-term joint damage in both conditions.
Table of Comparison
| Aspect | Osteoarthritis (OA) | Rheumatoid Arthritis (RA) |
|---|---|---|
| Cause | Wear and tear of cartilage | Autoimmune inflammation of joints |
| Onset | Gradual, usually after 40 years | Rapid or gradual, can occur at any age |
| Joint involvement | Weight-bearing joints (knees, hips), hands | Small joints (fingers, wrists), symmetric |
| Symptoms | Pain with activity, stiffness less than 30 minutes | Morning stiffness over 60 minutes, swelling, fatigue |
| Inflammation | Minimal or absent | Significant and persistent inflammation |
| Systemic effects | None | Fever, weight loss, malaise |
| Laboratory markers | Normal ESR, CRP, rheumatoid factor negative | Elevated ESR, CRP, positive rheumatoid factor, anti-CCP antibodies |
| Radiology | Joint space narrowing, osteophytes | Marginal bone erosions, joint space narrowing |
| Treatment | Pain relief, physical therapy, joint replacement | Immunosuppressants, DMARDs, biologics |
| Prognosis | Chronic, progressive with joint damage | Variable, potential joint deformity if untreated |
Overview: Osteoarthritis vs Rheumatoid Arthritis
Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage, primarily affecting weight-bearing joints such as the knees, hips, and spine, leading to pain and stiffness. Rheumatoid arthritis is an autoimmune disorder causing inflammation of the synovial membrane, resulting in joint swelling, deformity, and systemic symptoms like fatigue. Both conditions cause joint pain but differ in pathophysiology, with osteoarthritis linked to mechanical wear and rheumatoid arthritis driven by immune system dysregulation.
Causes and Risk Factors
Osteoarthritis primarily results from the gradual wear and tear of cartilage due to aging, joint overuse, or injury, with risk factors including obesity, repetitive stress, and older age. Rheumatoid arthritis is an autoimmune disorder where the immune system attacks joint linings, influenced by genetic predisposition, environmental triggers like smoking, and hormonal changes. Both conditions involve joint inflammation but differ fundamentally in their underlying causes and associated risks.
Symptoms Comparison
Osteoarthritis primarily causes joint pain, stiffness, and swelling, typically affecting weight-bearing joints such as knees and hips, with symptoms worsening after activity. Rheumatoid arthritis presents with symmetrical joint swelling, prolonged morning stiffness lasting over an hour, and systemic symptoms like fatigue and fever. Joint deformities and nodules are more common in rheumatoid arthritis, while osteoarthritis tends to involve localized joint degeneration without systemic involvement.
Diagnosing Osteoarthritis and Rheumatoid Arthritis
Osteoarthritis diagnosis relies on clinical evaluation of joint pain, stiffness, and X-rays showing cartilage degradation and bone spurs, primarily in weight-bearing joints. Rheumatoid arthritis diagnosis involves detecting specific autoantibodies like rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies, along with blood markers of inflammation such as ESR and CRP. Imaging techniques like ultrasound or MRI can further identify synovial inflammation and joint erosion characteristic of rheumatoid arthritis.
Joint Affected: Similarities and Differences
Osteoarthritis primarily affects the cartilage in weight-bearing joints such as knees, hips, and spine, leading to joint stiffness and pain. Rheumatoid arthritis targets the synovial membrane of smaller joints, including hands, wrists, and feet, causing inflammation and joint deformity. Both conditions involve joint inflammation but differ in the specific tissues affected and the pattern of joint involvement.
Disease Progression and Prognosis
Osteoarthritis typically progresses gradually due to cartilage degeneration, leading to joint stiffness and pain, but rarely causes systemic symptoms, with a prognosis focused on symptom management and joint preservation. Rheumatoid arthritis is an autoimmune condition marked by chronic inflammation, potentially causing rapid joint damage, deformities, and systemic complications, requiring aggressive treatment to slow disease progression and improve long-term outcomes. Early diagnosis and tailored therapies significantly influence prognosis in both conditions, with rheumatoid arthritis often demanding more intensive intervention to prevent irreversible damage.
Treatment Options for Each Condition
Osteoarthritis treatment primarily involves pain management through nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, and lifestyle modifications like weight loss and low-impact exercise to reduce joint strain. Rheumatoid arthritis requires disease-modifying antirheumatic drugs (DMARDs), including methotrexate and biologics, to suppress the autoimmune response and prevent joint damage. Both conditions may benefit from corticosteroid injections and surgical interventions in advanced cases, but treatment protocols differ significantly based on the underlying pathology and disease progression.
Lifestyle Modifications and Self-Care
Osteoarthritis management emphasizes weight control, low-impact exercise such as swimming or cycling, and joint protection techniques to reduce pain and improve mobility. Rheumatoid arthritis requires tailored self-care including regular physical activity, stress reduction strategies, and adherence to prescribed medication to manage inflammation and prevent joint damage. Both conditions benefit from ergonomic adjustments, balanced nutrition, and consistent monitoring of symptoms to enhance quality of life.
Complications and Long-Term Effects
Osteoarthritis primarily leads to joint stiffness, decreased mobility, and chronic pain due to cartilage degeneration, often resulting in osteophyte formation and joint deformity. Rheumatoid arthritis, an autoimmune disorder, causes systemic inflammation that can lead to joint erosion, deformities, and complications such as cardiovascular disease, lung fibrosis, and increased risk of osteoporosis. Both conditions can result in significant disability, but rheumatoid arthritis is associated with more severe systemic complications and long-term organ involvement.
Prevention Strategies and Early Detection
Osteoarthritis prevention focuses on maintaining joint health through regular low-impact exercise, weight management, and avoiding joint injuries, while rheumatoid arthritis prevention emphasizes early immune system regulation and monitoring genetic risk factors. Early detection of osteoarthritis involves identifying joint pain and stiffness through imaging techniques such as X-rays or MRI, whereas rheumatoid arthritis requires blood tests detecting specific antibodies like rheumatoid factor (RF) and anti-CCP for timely diagnosis. Implementing targeted screening and lifestyle modifications can significantly reduce the progression and severity of both conditions.
Osteoarthritis vs Rheumatoid arthritis Infographic
 difterm.com
difterm.com