MACs (microbiota-accessible carbohydrates) support gut health by nourishing beneficial bacteria and promoting a diverse microbiome, while FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) can trigger digestive discomfort in sensitive individuals due to their fermentable nature. Incorporating MACs into the diet encourages microbial fermentation that produces short-chain fatty acids, essential for colon integrity and immune function. Managing FODMAP intake helps reduce symptoms like bloating and gas, but overly restrictive diets may limit MACs and negatively impact microbiota diversity.
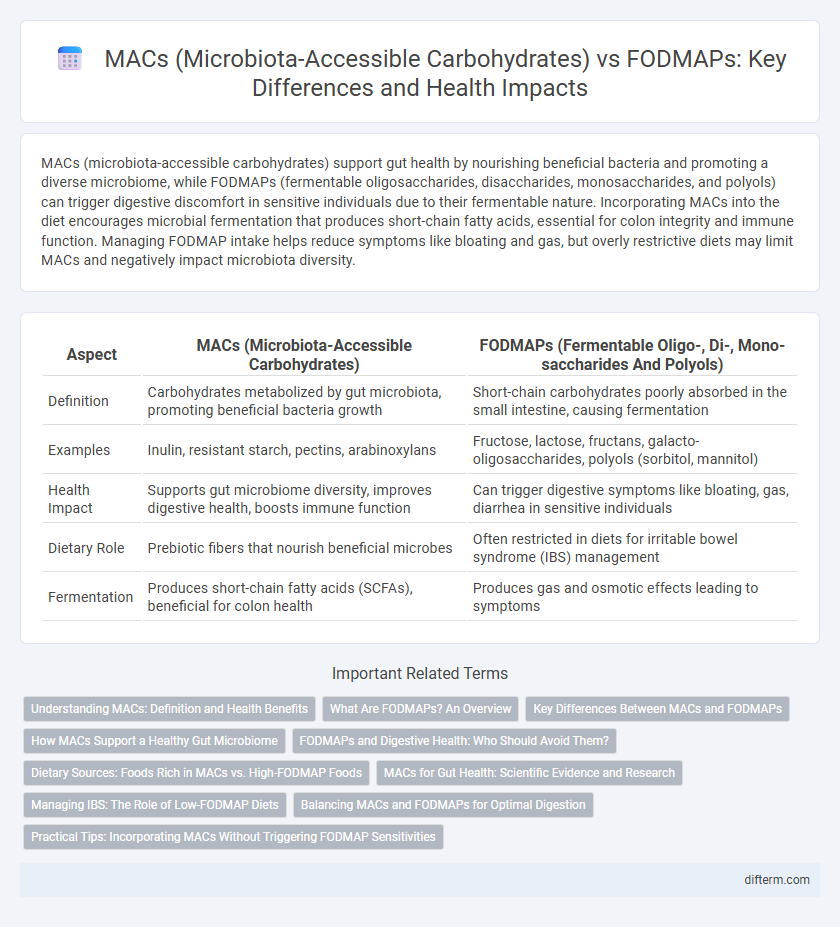
Table of Comparison
| Aspect | MACs (Microbiota-Accessible Carbohydrates) | FODMAPs (Fermentable Oligo-, Di-, Mono-saccharides And Polyols) |
|---|---|---|
| Definition | Carbohydrates metabolized by gut microbiota, promoting beneficial bacteria growth | Short-chain carbohydrates poorly absorbed in the small intestine, causing fermentation |
| Examples | Inulin, resistant starch, pectins, arabinoxylans | Fructose, lactose, fructans, galacto-oligosaccharides, polyols (sorbitol, mannitol) |
| Health Impact | Supports gut microbiome diversity, improves digestive health, boosts immune function | Can trigger digestive symptoms like bloating, gas, diarrhea in sensitive individuals |
| Dietary Role | Prebiotic fibers that nourish beneficial microbes | Often restricted in diets for irritable bowel syndrome (IBS) management |
| Fermentation | Produces short-chain fatty acids (SCFAs), beneficial for colon health | Produces gas and osmotic effects leading to symptoms |
Understanding MACs: Definition and Health Benefits
Microbiota-accessible carbohydrates (MACs) are dietary fibers that resist digestion in the small intestine and undergo fermentation by gut microbiota, producing short-chain fatty acids essential for colon health. Unlike FODMAPs, which can trigger digestive discomfort in sensitive individuals, MACs promote microbial diversity and enhance gut barrier function. Increasing MAC intake supports immune modulation, reduces inflammation, and improves metabolic health through a well-nourished microbiome.
What Are FODMAPs? An Overview
FODMAPs are a group of fermentable short-chain carbohydrates that include oligosaccharides, disaccharides, monosaccharides, and polyols, which can cause digestive issues in sensitive individuals. Unlike MACs (microbiota-accessible carbohydrates) that nourish beneficial gut bacteria, FODMAPs often lead to gas, bloating, and abdominal pain due to poor absorption in the small intestine. Understanding FODMAPs is crucial for managing conditions like irritable bowel syndrome (IBS) through tailored dietary interventions.
Key Differences Between MACs and FODMAPs
MACs (microbiota-accessible carbohydrates) are dietary fibers that specifically nourish beneficial gut bacteria, promoting microbial diversity and long-term gut health. FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) are short-chain carbohydrates that can cause digestive discomfort in sensitive individuals due to rapid fermentation and gas production. Unlike FODMAPs, which may need to be limited in conditions like irritable bowel syndrome (IBS), MACs are generally encouraged to support a balanced and resilient microbiome.
How MACs Support a Healthy Gut Microbiome
Microbiota-accessible carbohydrates (MACs) serve as essential fuel for beneficial gut bacteria, promoting microbial diversity and synthesis of short-chain fatty acids like butyrate, which support gut barrier integrity and reduce inflammation. Unlike FODMAPs, which are fermentable oligosaccharides linked to digestive discomfort in sensitive individuals, MACs enhance overall gut health by fostering a balanced and resilient microbiome. Increased intake of MACs from sources such as legumes, whole grains, and fruits directly contributes to improved digestion and metabolic function.
FODMAPs and Digestive Health: Who Should Avoid Them?
FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) are short-chain carbohydrates that can trigger digestive symptoms like bloating, gas, and abdominal pain in individuals with irritable bowel syndrome (IBS) or small intestinal bacterial overgrowth (SIBO). People with sensitive digestive systems, including those diagnosed with IBS, often benefit from limiting FODMAP intake to reduce inflammation and improve gut motility. Unlike microbiota-accessible carbohydrates (MACs) that promote healthy microbial diversity, restricting FODMAPs helps manage digestive discomfort by minimizing fermentation-related distress in susceptible populations.
Dietary Sources: Foods Rich in MACs vs. High-FODMAP Foods
Foods rich in microbiota-accessible carbohydrates (MACs) include whole grains, legumes, fruits like apples and berries, and vegetables such as artichokes and asparagus, which promote gut microbiota diversity and short-chain fatty acid production. High-FODMAP foods, including garlic, onions, wheat, and certain dairy products, contain fermentable oligosaccharides, disaccharides, monosaccharides, and polyols that can trigger gastrointestinal symptoms in sensitive individuals. Choosing MAC-rich foods supports a healthy gut environment, whereas limiting high-FODMAP foods is often necessary for managing irritable bowel syndrome (IBS) symptoms.
MACs for Gut Health: Scientific Evidence and Research
Microbiota-accessible carbohydrates (MACs) serve as essential substrates for the gut microbiota, promoting microbial diversity and short-chain fatty acid production, crucial for maintaining intestinal barrier integrity and immune function. Scientific studies demonstrate that MACs enhance gut health by fostering beneficial bacterial growth and reducing inflammation, contrasting with FODMAPs, which may exacerbate symptoms in sensitive individuals despite their fermentability. Research underscores the importance of MACs in supporting a resilient microbiome, highlighting their role in preventing dysbiosis and associated gastrointestinal disorders.
Managing IBS: The Role of Low-FODMAP Diets
Managing IBS effectively often involves a low-FODMAP diet, which restricts fermentable oligosaccharides, disaccharides, monosaccharides, and polyols known to exacerbate symptoms. Microbiota-accessible carbohydrates (MACs) differ as they promote gut microbiome diversity and overall digestive health, contrasting with FODMAPs that may trigger IBS flare-ups. Balancing low-FODMAP intake while ensuring adequate MAC consumption supports symptom relief without compromising beneficial microbial nutrition.
Balancing MACs and FODMAPs for Optimal Digestion
Balancing microbiota-accessible carbohydrates (MACs) and FODMAPs is crucial for optimal digestion and gut health, as MACs nourish beneficial gut bacteria while FODMAPs can trigger digestive discomfort in sensitive individuals. Incorporating a diverse intake of MAC-rich foods like whole grains, legumes, and vegetables supports microbial diversity, whereas moderating high-FODMAP foods such as garlic, onions, and wheat helps manage symptoms of irritable bowel syndrome (IBS). Tailoring the diet to individual tolerance levels ensures effective fermentation processes without exacerbating gastrointestinal distress.
Practical Tips: Incorporating MACs Without Triggering FODMAP Sensitivities
Incorporate microbiota-accessible carbohydrates (MACs) by selecting low-FODMAP sources such as unripe bananas, oats, and peeled carrots to nourish gut bacteria without causing digestive distress. Gradual introduction of MACs allows the microbiome to adapt, minimizing symptoms associated with FODMAP sensitivities like bloating and gas. Monitoring portion sizes and using a personalized FODMAP app can help balance gut health benefits while avoiding fermentation-related discomfort.
MACs (microbiota-accessible carbohydrates) vs FODMAPs Infographic
 difterm.com
difterm.com