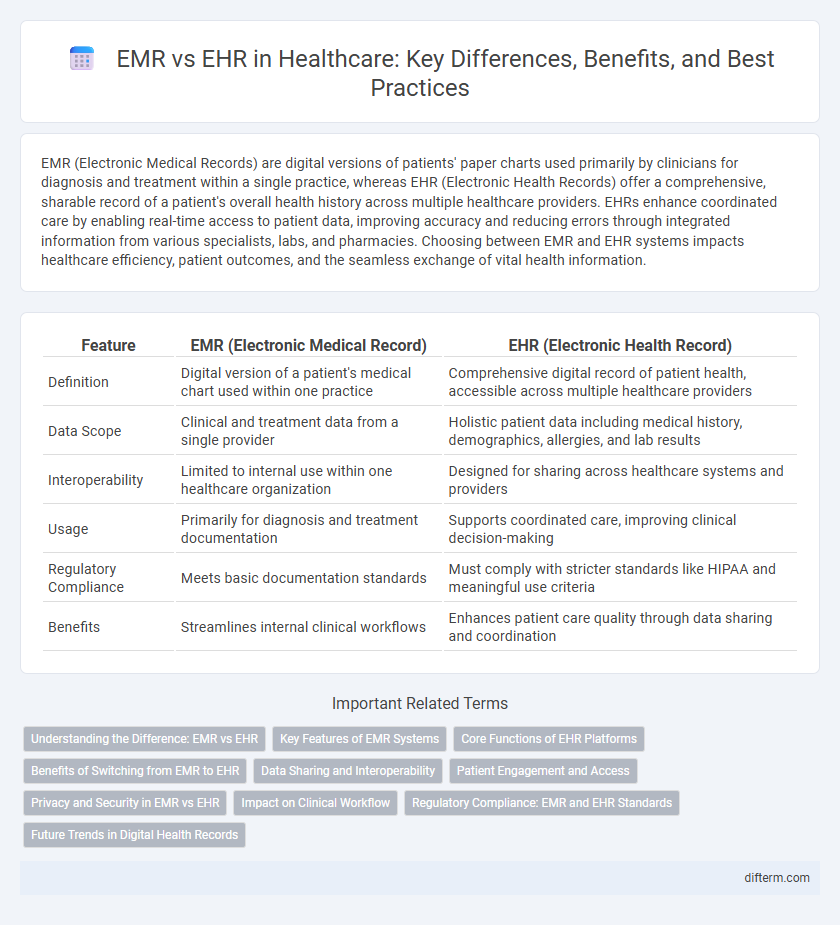
EMR (Electronic Medical Records) are digital versions of patients' paper charts used primarily by clinicians for diagnosis and treatment within a single practice, whereas EHR (Electronic Health Records) offer a comprehensive, sharable record of a patient's overall health history across multiple healthcare providers. EHRs enhance coordinated care by enabling real-time access to patient data, improving accuracy and reducing errors through integrated information from various specialists, labs, and pharmacies. Choosing between EMR and EHR systems impacts healthcare efficiency, patient outcomes, and the seamless exchange of vital health information.
Table of Comparison
| Feature | EMR (Electronic Medical Record) | EHR (Electronic Health Record) |
|---|---|---|
| Definition | Digital version of a patient's medical chart used within one practice | Comprehensive digital record of patient health, accessible across multiple healthcare providers |
| Data Scope | Clinical and treatment data from a single provider | Holistic patient data including medical history, demographics, allergies, and lab results |
| Interoperability | Limited to internal use within one healthcare organization | Designed for sharing across healthcare systems and providers |
| Usage | Primarily for diagnosis and treatment documentation | Supports coordinated care, improving clinical decision-making |
| Regulatory Compliance | Meets basic documentation standards | Must comply with stricter standards like HIPAA and meaningful use criteria |
| Benefits | Streamlines internal clinical workflows | Enhances patient care quality through data sharing and coordination |
Understanding the Difference: EMR vs EHR
Electronic Medical Records (EMR) are digital versions of a patient's paper charts within a single healthcare practice, primarily used for diagnosis and treatment. Electronic Health Records (EHR) encompass a broader scope, aggregating comprehensive health information from multiple providers to support coordinated patient care across different healthcare settings. Understanding the difference enhances healthcare interoperability and improves patient outcomes by facilitating seamless information exchange.
Key Features of EMR Systems
Electronic Medical Records (EMR) systems feature digital versions of patients' paper charts, designed primarily for use within a single healthcare organization to streamline clinical workflows. Key features include real-time patient data tracking, integration with laboratory and imaging results, and tools for clinical decision support that enhance diagnostics and treatment plans. EMRs also improve documentation accuracy, facilitate secure information sharing among physicians, and support compliance with healthcare regulations, ultimately increasing operational efficiency.
Core Functions of EHR Platforms
EHR platforms offer core functions such as comprehensive patient data management, including medical history, medication lists, and immunization records, which support coordinated care across multiple providers. They facilitate clinical decision support with alerts and reminders, enhancing diagnostic accuracy and treatment effectiveness. Interoperability features enable seamless information exchange across healthcare systems, improving patient outcomes and operational efficiency.
Benefits of Switching from EMR to EHR
Switching from EMR to EHR enhances patient care through comprehensive data sharing across healthcare providers, improving diagnosis and treatment accuracy. EHR systems support interoperability, allowing seamless communication among specialists, labs, and pharmacies, which streamlines workflows and reduces medical errors. Enhanced data analytics in EHRs enable personalized medicine and population health management, leading to better health outcomes and increased efficiency.
Data Sharing and Interoperability
Electronic Medical Records (EMR) primarily store patient data within a single practice, limiting data sharing capabilities and interoperability across different healthcare providers. Electronic Health Records (EHR) facilitate seamless data exchange and integration across multiple healthcare systems, enhancing coordinated patient care and clinical decision-making. Advanced interoperability standards like HL7 FHIR support EHR systems by enabling real-time access to comprehensive patient information across diverse platforms.
Patient Engagement and Access
Electronic Medical Records (EMR) primarily serve healthcare providers by digitizing patient charts, while Electronic Health Records (EHR) offer broader access, enabling patients to securely view their health information across multiple providers. EHR systems enhance patient engagement by providing tools such as appointment scheduling, test result access, and direct communication with care teams. Improved accessibility through EHR platforms promotes informed decision-making and empowers patients to take an active role in managing their health.
Privacy and Security in EMR vs EHR
Electronic Medical Records (EMR) are primarily designed for use within a single healthcare organization, which limits data sharing but enhances control over patient privacy through localized security measures. Electronic Health Records (EHR) support broader interoperability across multiple healthcare providers, increasing the exposure to security risks yet enabling comprehensive patient data exchange with advanced encryption and access controls. Prioritizing robust cybersecurity protocols, EHR systems implement multi-factor authentication and audit trails to protect sensitive information, whereas EMRs rely on internal network protections and limited user access to maintain privacy integrity.
Impact on Clinical Workflow
EMR systems streamline clinical workflow by digitizing patient charts, enabling faster documentation and easier access to medical histories within a single practice. EHR platforms enhance workflow efficiency across multiple healthcare settings by facilitating seamless data sharing, improving coordination among specialists, and supporting comprehensive care management. Both systems reduce administrative burdens and minimize errors, but EHRs offer broader interoperability, which significantly impacts clinical decision-making and patient outcomes.
Regulatory Compliance: EMR and EHR Standards
EMR systems primarily focus on meeting healthcare provider requirements while adhering to HIPAA regulations for secure patient data storage, whereas EHR standards emphasize interoperability and compliance with broader regulatory frameworks like ONC's Cures Act Final Rule. Both EMR and EHR must ensure data accuracy, confidentiality, and accessibility, aligning with Meaningful Use criteria and CMS requirements to support quality care and reporting. Regulatory compliance drives continuous updates in certification processes, ensuring that these health IT systems adhere to evolving federal and state mandates.
Future Trends in Digital Health Records
Emerging future trends in digital health records emphasize the integration of Electronic Medical Records (EMR) with Electronic Health Records (EHR) to enhance interoperability and patient-centered care. Advanced technologies like artificial intelligence and blockchain are poised to improve data accuracy, security, and real-time health analytics. These innovations aim to transform healthcare by enabling seamless data exchange across providers, fostering personalized treatment plans, and supporting telehealth expansion.
EMR vs EHR Infographic
 difterm.com
difterm.com