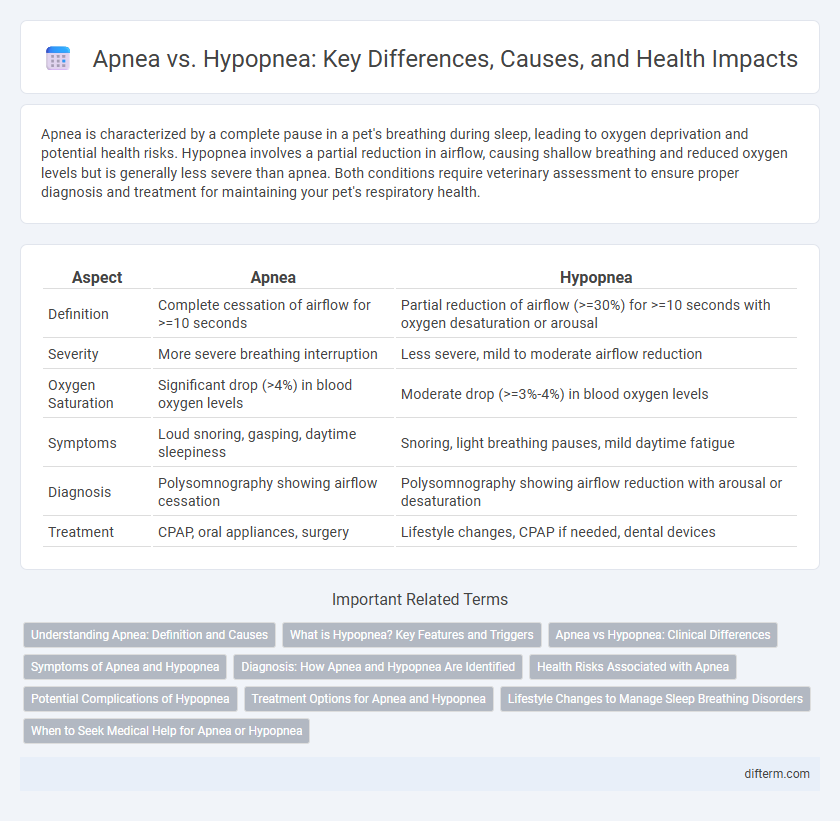
Apnea is characterized by a complete pause in a pet's breathing during sleep, leading to oxygen deprivation and potential health risks. Hypopnea involves a partial reduction in airflow, causing shallow breathing and reduced oxygen levels but is generally less severe than apnea. Both conditions require veterinary assessment to ensure proper diagnosis and treatment for maintaining your pet's respiratory health.
Table of Comparison
| Aspect | Apnea | Hypopnea |
|---|---|---|
| Definition | Complete cessation of airflow for >=10 seconds | Partial reduction of airflow (>=30%) for >=10 seconds with oxygen desaturation or arousal |
| Severity | More severe breathing interruption | Less severe, mild to moderate airflow reduction |
| Oxygen Saturation | Significant drop (>4%) in blood oxygen levels | Moderate drop (>=3%-4%) in blood oxygen levels |
| Symptoms | Loud snoring, gasping, daytime sleepiness | Snoring, light breathing pauses, mild daytime fatigue |
| Diagnosis | Polysomnography showing airflow cessation | Polysomnography showing airflow reduction with arousal or desaturation |
| Treatment | CPAP, oral appliances, surgery | Lifestyle changes, CPAP if needed, dental devices |
Understanding Apnea: Definition and Causes
Apnea is characterized by a complete cessation of airflow for at least 10 seconds during sleep, often caused by obstruction of the upper airway or neurological factors disrupting respiratory signals. Understanding apnea involves recognizing its triggers, such as obesity, anatomical abnormalities, and central nervous system disorders, which impair breathing regulation. The severity and frequency of apnea episodes directly impact oxygen saturation and sleep quality, differentiating it from hypopnea, which involves partial airflow reduction.
What is Hypopnea? Key Features and Triggers
Hypopnea is a sleep disorder characterized by partial obstruction of the airway, resulting in shallow or slow breathing during sleep and reduced oxygen levels in the blood. Key features include a decrease in airflow by at least 30% for 10 seconds or longer, accompanied by oxygen desaturation or arousal from sleep. Common triggers involve obesity, nasal congestion, alcohol consumption, and anatomical abnormalities such as enlarged tonsils or a deviated septum.
Apnea vs Hypopnea: Clinical Differences
Apnea involves a complete cessation of airflow lasting at least 10 seconds, while hypopnea is characterized by a partial reduction in airflow accompanied by oxygen desaturation or arousal from sleep. Clinically, apnea results in more severe oxygen desaturation and greater sleep fragmentation compared to hypopnea, often leading to more pronounced daytime sleepiness and cardiovascular risk. Polysomnography is essential for differentiating these events, as apnea episodes typically correlate with higher apnea-hypopnea index (AHI) scores indicative of obstructive sleep apnea severity.
Symptoms of Apnea and Hypopnea
Apnea is characterized by repeated pauses in breathing lasting at least 10 seconds, often causing loud snoring, gasping, and excessive daytime sleepiness. Hypopnea involves shallow or slow breathing that reduces airflow by 30-50%, leading to disrupted sleep, fatigue, and morning headaches. Both conditions may contribute to restless sleep patterns and cardiovascular issues if left untreated.
Diagnosis: How Apnea and Hypopnea Are Identified
Apnea is diagnosed through polysomnography by detecting complete pauses in airflow lasting at least 10 seconds, while hypopnea is identified by partial reductions in airflow accompanied by oxygen desaturation or arousal. The Apnea-Hypopnea Index (AHI) quantifies severity by calculating the average number of apnea and hypopnea events per hour of sleep. Oxygen saturation levels and sleep stage disruptions provide critical data for distinguishing between apnea and hypopnea during diagnosis.
Health Risks Associated with Apnea
Apnea involves complete pauses in breathing during sleep, significantly increasing the risk of cardiovascular diseases, hypertension, stroke, and daytime fatigue due to oxygen deprivation. Hypopnea is characterized by partial airway obstruction leading to shallow breathing, which poses fewer but still serious health risks such as reduced oxygen levels and disturbed sleep patterns. Untreated apnea results in more severe health complications compared to hypopnea, emphasizing the need for early diagnosis and treatment.
Potential Complications of Hypopnea
Hypopnea, characterized by partial airway obstruction leading to reduced airflow during sleep, can result in decreased oxygen levels and fragmented sleep. Potential complications include increased risk of cardiovascular diseases such as hypertension, arrhythmias, and stroke due to chronic intermittent hypoxia. Moreover, untreated hypopnea may contribute to daytime fatigue, cognitive impairment, and metabolic disorders like type 2 diabetes.
Treatment Options for Apnea and Hypopnea
Treatment options for apnea primarily include the use of continuous positive airway pressure (CPAP) devices, which maintain open airways during sleep, while hypopnea is often managed with lifestyle changes such as weight loss and positional therapy. Oral appliances that reposition the jaw to improve airflow can be effective for both conditions, especially in mild to moderate cases. In more severe instances, surgical interventions like uvulopalatopharyngoplasty (UPPP) or hypoglossal nerve stimulation may be recommended to reduce airway obstruction.
Lifestyle Changes to Manage Sleep Breathing Disorders
Lifestyle changes play a critical role in managing sleep breathing disorders such as apnea and hypopnea. Weight loss, regular exercise, and avoiding alcohol or sedatives before bedtime can reduce airway obstruction and improve breathing quality. Establishing consistent sleep routines and sleeping on one's side also helps minimize episodes of interrupted airflow during sleep.
When to Seek Medical Help for Apnea or Hypopnea
Seek medical help for apnea or hypopnea if you experience frequent pauses in breathing, loud snoring, or excessive daytime sleepiness, which can indicate obstructive sleep apnea. Persistent episodes of shallow breathing or interrupted airflow during sleep may lead to serious complications like cardiovascular disease or cognitive impairment. Early diagnosis and treatment through a sleep study can prevent long-term health risks and improve overall sleep quality.
Apnea vs Hypopnea Infographic
 difterm.com
difterm.com