The gut-brain axis involves a complex communication network where gut microbiota influence neurological health and behavior through signaling pathways such as the vagus nerve and immune modulation. In contrast, the gut-liver axis primarily regulates metabolic processes and detoxification, with gut-derived metabolites affecting liver function and contributing to conditions like fatty liver disease. Understanding these distinct pathways is crucial for developing targeted interventions to improve overall pet health by modulating gut microbiota.
Table of Comparison
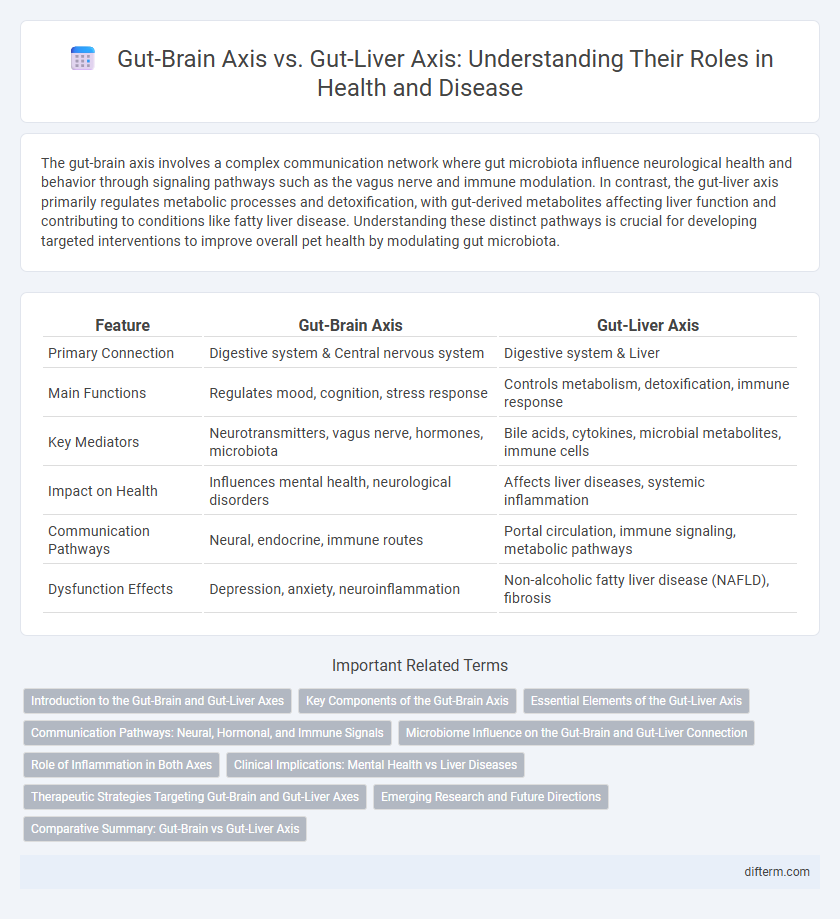
| Feature | Gut-Brain Axis | Gut-Liver Axis |
|---|---|---|
| Primary Connection | Digestive system & Central nervous system | Digestive system & Liver |
| Main Functions | Regulates mood, cognition, stress response | Controls metabolism, detoxification, immune response |
| Key Mediators | Neurotransmitters, vagus nerve, hormones, microbiota | Bile acids, cytokines, microbial metabolites, immune cells |
| Impact on Health | Influences mental health, neurological disorders | Affects liver diseases, systemic inflammation |
| Communication Pathways | Neural, endocrine, immune routes | Portal circulation, immune signaling, metabolic pathways |
| Dysfunction Effects | Depression, anxiety, neuroinflammation | Non-alcoholic fatty liver disease (NAFLD), fibrosis |
Introduction to the Gut-Brain and Gut-Liver Axes
The gut-brain axis is a complex communication network linking the central nervous system with the enteric nervous system, influencing digestion, mood, and cognitive functions through neural, hormonal, and immune pathways. The gut-liver axis involves bidirectional interactions between the gut microbiota and liver, impacting metabolic processes, immune responses, and detoxification via the portal vein and bile acids. Understanding these axes reveals how gut health affects systemic diseases, including neurodegenerative disorders and liver conditions like non-alcoholic fatty liver disease (NAFLD).
Key Components of the Gut-Brain Axis
The gut-brain axis involves key components such as the enteric nervous system, vagus nerve, immune system, and gut microbiota, facilitating bidirectional communication between the gastrointestinal tract and central nervous system. Neurotransmitters produced in the gut, including serotonin and gamma-aminobutyric acid (GABA), play critical roles in modulating mood and cognitive functions. This complex network contrasts with the gut-liver axis, which primarily involves metabolic and immunological interactions affecting liver function and systemic inflammation.
Essential Elements of the Gut-Liver Axis
The gut-liver axis is a critical bidirectional communication system involving the portal vein, bile acids, and immune signaling pathways that regulate metabolic homeostasis and inflammatory responses. Essential elements include the intestinal barrier, microbiota-derived metabolites, and hepatic immune cells, which collectively influence liver function and systemic health. Dysregulation within this axis contributes to liver diseases such as non-alcoholic fatty liver disease (NAFLD) and alcoholic liver disease (ALD).
Communication Pathways: Neural, Hormonal, and Immune Signals
The gut-brain axis and gut-liver axis communicate through complex neural, hormonal, and immune pathways that regulate physiological homeostasis. The gut-brain axis primarily utilizes the vagus nerve and enteric nervous system for bidirectional neural signaling, coupled with hormonal signals like serotonin and glucagon-like peptide-1, while immune mediators such as cytokines influence neuroinflammation. Conversely, the gut-liver axis relies on portal vein blood flow to transport microbial metabolites and hormones directly to the liver, with immune pathways modulating hepatic inflammation and metabolic responses.
Microbiome Influence on the Gut-Brain and Gut-Liver Connection
The gut microbiome plays a critical role in modulating both the gut-brain and gut-liver axes by producing metabolites like short-chain fatty acids, neurotransmitters, and bile acids that influence neural signaling and liver function. Dysbiosis in the gut microbiome has been linked to neuroinflammatory conditions, cognitive disorders through the gut-brain axis, and hepatic diseases including non-alcoholic fatty liver disease via the gut-liver axis. Targeting microbiome composition through probiotics, prebiotics, or dietary interventions offers promising therapeutic potential for restoring homeostasis in both neural and hepatic pathways.
Role of Inflammation in Both Axes
Inflammation plays a critical role in modulating the communication between the gut-brain axis and gut-liver axis, influencing systemic health outcomes. In the gut-brain axis, neuroinflammation triggered by gut microbiota imbalance can affect mood disorders and neurodegenerative diseases. In the gut-liver axis, inflammation driven by gut-derived endotoxins contributes to liver diseases such as non-alcoholic fatty liver disease (NAFLD) and cirrhosis, highlighting the importance of immune responses in both regulatory pathways.
Clinical Implications: Mental Health vs Liver Diseases
The gut-brain axis is critically involved in mental health disorders such as depression, anxiety, and neurodegenerative diseases, with alterations in gut microbiota influencing neurotransmitter production and inflammatory pathways. In contrast, the gut-liver axis plays a pivotal role in liver diseases, including non-alcoholic fatty liver disease (NAFLD) and cirrhosis, through microbial metabolites and immune responses impacting liver inflammation and fibrosis. Understanding these distinct axes provides targeted clinical strategies for managing neuropsychiatric conditions and hepatic pathologies by modulating gut microbiota and gut-derived signals.
Therapeutic Strategies Targeting Gut-Brain and Gut-Liver Axes
Therapeutic strategies targeting the gut-brain axis primarily focus on modulating microbiota composition and signaling pathways to alleviate neurological and psychiatric disorders such as depression, anxiety, and autism spectrum disorders. Interventions for the gut-liver axis aim to restore intestinal barrier function and reduce hepatic inflammation in conditions like non-alcoholic fatty liver disease (NAFLD) and cirrhosis by using probiotics, prebiotics, and bile acid modulators. Precision medicine approaches harness gut microbiome profiling and metabolomics to tailor treatments that simultaneously address both axes, improving systemic metabolic and inflammatory outcomes.
Emerging Research and Future Directions
Emerging research on the gut-brain axis highlights the complex bidirectional communication between the central nervous system and gut microbiota, influencing neurological disorders such as anxiety, depression, and neurodegenerative diseases. Meanwhile, studies on the gut-liver axis reveal critical interactions affecting liver diseases like non-alcoholic fatty liver disease (NAFLD) through microbial metabolites and immune responses. Future directions emphasize microbiome-targeted therapies, including probiotics, prebiotics, and fecal microbiota transplantation, aiming to modulate these axes for improved neuropsychiatric and hepatic health outcomes.
Comparative Summary: Gut-Brain vs Gut-Liver Axis
The gut-brain axis primarily regulates neurological and psychological functions through bidirectional communication involving the vagus nerve, neurotransmitters, and microbial metabolites, influencing stress, mood, and cognitive processes. Conversely, the gut-liver axis focuses on metabolic regulation and immune responses, where gut-derived substances such as lipopolysaccharides and bile acids impact liver inflammation, detoxification, and systemic metabolism. Both axes share microbial interactions but differ in target organs and physiological outcomes, highlighting distinct pathways crucial for maintaining brain and liver health respectively.
Gut-brain axis vs Gut-liver axis Infographic
 difterm.com
difterm.com