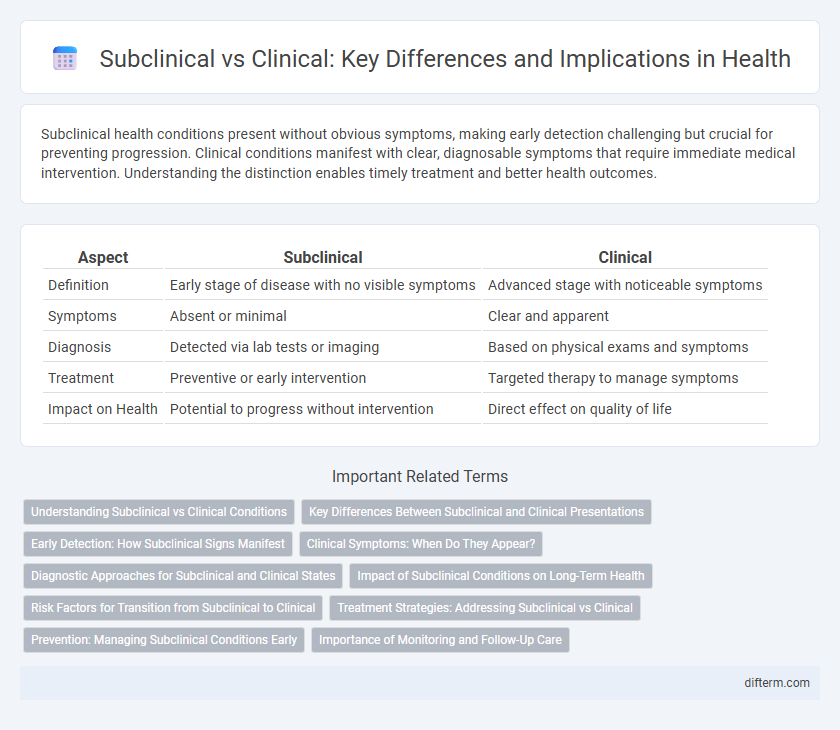
Subclinical health conditions present without obvious symptoms, making early detection challenging but crucial for preventing progression. Clinical conditions manifest with clear, diagnosable symptoms that require immediate medical intervention. Understanding the distinction enables timely treatment and better health outcomes.
Table of Comparison
| Aspect | Subclinical | Clinical |
|---|---|---|
| Definition | Early stage of disease with no visible symptoms | Advanced stage with noticeable symptoms |
| Symptoms | Absent or minimal | Clear and apparent |
| Diagnosis | Detected via lab tests or imaging | Based on physical exams and symptoms |
| Treatment | Preventive or early intervention | Targeted therapy to manage symptoms |
| Impact on Health | Potential to progress without intervention | Direct effect on quality of life |
Understanding Subclinical vs Clinical Conditions
Subclinical conditions exhibit biological or physiological abnormalities without visible symptoms, making early detection reliant on diagnostic tests rather than clinical presentation. Clinical conditions manifest clear signs and symptoms that affect patient well-being, often prompting immediate medical attention and intervention. Differentiating between subclinical and clinical states is crucial for timely diagnosis and effective management to prevent progression and complications.
Key Differences Between Subclinical and Clinical Presentations
Subclinical presentations involve subtle or no obvious symptoms despite pathological changes, often detected only through laboratory tests or imaging studies. Clinical presentations exhibit clear, recognizable symptoms and signs that prompt medical diagnosis and treatment. Key differences include the severity of symptoms, detectability by routine examination, and the impact on daily functioning.
Early Detection: How Subclinical Signs Manifest
Subclinical signs manifest as subtle physiological changes or biomarkers that indicate the early onset of disease before symptoms become apparent, enabling proactive health interventions. For example, elevated blood pressure without symptoms can signal prehypertension, which may progress to clinical hypertension if untreated. Early detection through subclinical indicators improves patient outcomes by allowing timely lifestyle modifications and medical management.
Clinical Symptoms: When Do They Appear?
Clinical symptoms typically appear after a subclinical phase where signs are not yet detectable or are mild, indicating the disease has progressed to a more advanced stage. The onset of clinical symptoms varies depending on the condition but often emerges once pathological changes reach a threshold that affects normal bodily functions. Early recognition of these symptoms is crucial for timely diagnosis and effective treatment to prevent further complications.
Diagnostic Approaches for Subclinical and Clinical States
Diagnostic approaches for subclinical states rely heavily on sensitive biomarker assays, imaging techniques, and laboratory tests to detect early pathological changes before symptoms manifest. In clinical states, diagnosis is primarily based on symptomatic evaluation supported by confirmatory tests such as biopsies, electrophysiological studies, or advanced imaging that reveal overt disease. Early detection in subclinical stages enables intervention to prevent progression, while clinical diagnostics guide treatment strategies based on established disease presentation.
Impact of Subclinical Conditions on Long-Term Health
Subclinical conditions, characterized by the absence of overt symptoms, can silently contribute to the progression of chronic diseases such as hypertension, diabetes, and cardiovascular disorders. Early detection through biomarkers and advanced screening techniques enables intervention before clinical symptoms manifest, reducing long-term morbidity and healthcare costs. Ignoring subclinical stages often leads to irreversible organ damage and significantly worsened health outcomes over time.
Risk Factors for Transition from Subclinical to Clinical
Risk factors for the transition from subclinical to clinical stages include genetic predisposition, chronic inflammation, and environmental exposures such as smoking or pollutants. Elevated biomarkers like C-reactive protein (CRP) and specific autoantibodies increase the likelihood of disease progression. Early identification and monitoring of these risk factors enhance the potential for timely intervention and improved patient outcomes.
Treatment Strategies: Addressing Subclinical vs Clinical
Treatment strategies for subclinical conditions emphasize early intervention through lifestyle modifications and monitoring to prevent progression, whereas clinical conditions require more intensive therapies including pharmacological treatments and specialized medical procedures. Subclinical phase management often involves regular screenings and risk factor control to mitigate symptom development, while clinical management demands tailored medication plans and potentially surgical interventions to address overt disease manifestations. Effective differentiation between subclinical and clinical stages is critical for optimizing healthcare outcomes and allocating appropriate resources.
Prevention: Managing Subclinical Conditions Early
Managing subclinical conditions early involves regular screenings and biometric monitoring to detect subtle physiological changes before symptoms emerge. Intervention strategies targeting lifestyle modifications, such as improved diet, exercise, and stress reduction, can effectively prevent progression to clinical disease states. Proactive management of subclinical abnormalities reduces healthcare costs and enhances long-term patient outcomes by mitigating risk factors for chronic illnesses.
Importance of Monitoring and Follow-Up Care
Regular monitoring and follow-up care are crucial for managing both subclinical and clinical conditions, ensuring early detection of disease progression and timely intervention. Clinical assessments, laboratory tests, and imaging help track subtle changes in subclinical stages, preventing complications and improving long-term outcomes. Consistent follow-up fosters patient adherence, optimizing treatment efficacy and reducing the risk of chronic disease development.
Subclinical vs Clinical Infographic
 difterm.com
difterm.com