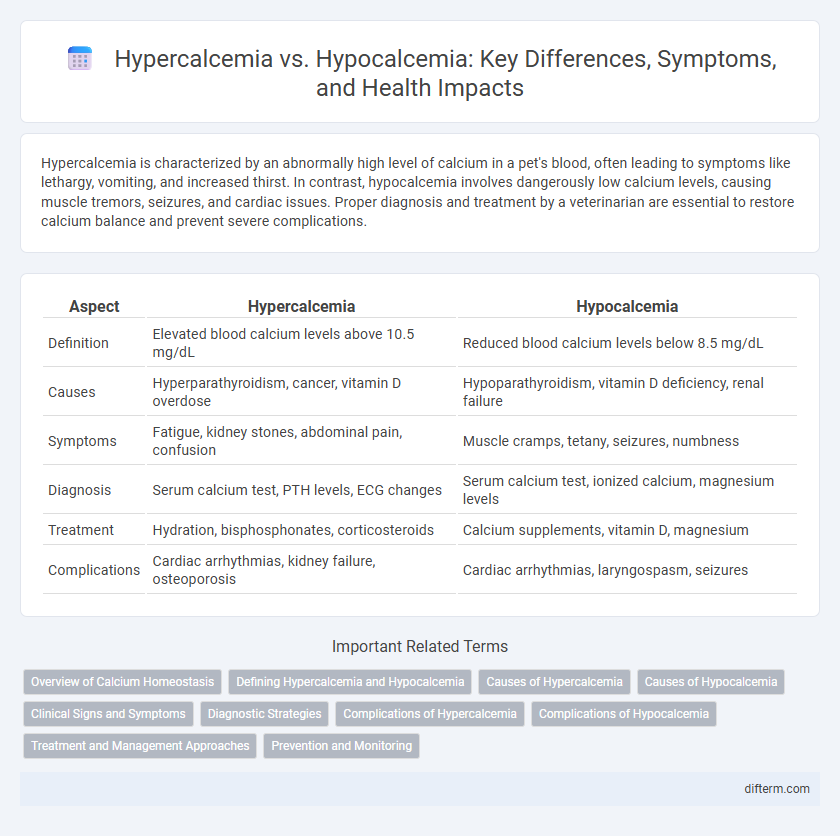
Hypercalcemia is characterized by an abnormally high level of calcium in a pet's blood, often leading to symptoms like lethargy, vomiting, and increased thirst. In contrast, hypocalcemia involves dangerously low calcium levels, causing muscle tremors, seizures, and cardiac issues. Proper diagnosis and treatment by a veterinarian are essential to restore calcium balance and prevent severe complications.
Table of Comparison
| Aspect | Hypercalcemia | Hypocalcemia |
|---|---|---|
| Definition | Elevated blood calcium levels above 10.5 mg/dL | Reduced blood calcium levels below 8.5 mg/dL |
| Causes | Hyperparathyroidism, cancer, vitamin D overdose | Hypoparathyroidism, vitamin D deficiency, renal failure |
| Symptoms | Fatigue, kidney stones, abdominal pain, confusion | Muscle cramps, tetany, seizures, numbness |
| Diagnosis | Serum calcium test, PTH levels, ECG changes | Serum calcium test, ionized calcium, magnesium levels |
| Treatment | Hydration, bisphosphonates, corticosteroids | Calcium supplements, vitamin D, magnesium |
| Complications | Cardiac arrhythmias, kidney failure, osteoporosis | Cardiac arrhythmias, laryngospasm, seizures |
Overview of Calcium Homeostasis
Calcium homeostasis maintains blood calcium levels between 8.5 and 10.5 mg/dL through a balance involving the parathyroid hormone (PTH), calcitonin, and vitamin D. Hypercalcemia results from excessive calcium due to increased bone resorption or decreased renal excretion, while hypocalcemia arises from insufficient calcium often caused by hypoparathyroidism or vitamin D deficiency. Proper regulation of calcium is critical for neuromuscular function, blood clotting, and skeletal integrity.
Defining Hypercalcemia and Hypocalcemia
Hypercalcemia is characterized by elevated calcium levels in the blood, typically above 10.5 mg/dL, leading to symptoms such as muscle weakness, fatigue, and kidney stones. Hypocalcemia refers to low blood calcium levels, usually below 8.5 mg/dL, causing muscle cramps, tetany, and cardiac arrhythmias. Both conditions disrupt calcium homeostasis, impacting bone health and neuromuscular function.
Causes of Hypercalcemia
Hypercalcemia occurs primarily due to hyperparathyroidism, malignancies such as lung or breast cancer, and excessive vitamin D intake. Other causes include certain medications like thiazide diuretics and prolonged immobilization, which increase calcium release from bones. Kidney failure and granulomatous diseases like sarcoidosis also contribute to elevated blood calcium levels.
Causes of Hypocalcemia
Hypocalcemia primarily results from vitamin D deficiency, impaired parathyroid hormone production, or chronic kidney disease, all disrupting calcium absorption and regulation. Other causes include magnesium deficiency, which impairs PTH secretion, and acute pancreatitis that leads to calcium binding and decreased serum levels. Understanding these factors is crucial for accurate diagnosis and effective treatment of hypocalcemia.
Clinical Signs and Symptoms
Hypercalcemia presents with clinical signs such as muscle weakness, fatigue, polyuria, and nausea, often accompanied by confusion or altered mental status in severe cases. Hypocalcemia symptoms include tetany, paresthesia, muscle spasms, and seizures, frequently triggered by low serum calcium levels affecting neuromuscular excitability. Both conditions require prompt diagnosis through serum calcium measurement and management to prevent complications like cardiac arrhythmias or neurological deficits.
Diagnostic Strategies
Accurate diagnosis of hypercalcemia involves measuring serum calcium levels, parathyroid hormone (PTH), and 24-hour urine calcium to differentiate primary hyperparathyroidism from malignancy-induced causes. Hypocalcemia diagnosis requires assessing total and ionized calcium, serum albumin, magnesium, phosphate levels, and PTH to identify underlying conditions such as hypoparathyroidism or vitamin D deficiency. Advanced imaging, including neck ultrasound and sestamibi scan, supports hypercalcemia workup, while ECG changes help in detecting hypocalcemia severity.
Complications of Hypercalcemia
Hypercalcemia, characterized by elevated calcium levels in the blood, can lead to severe complications such as kidney stones, nephrocalcinosis, and impaired renal function. Prolonged hypercalcemia increases the risk of cardiac arrhythmias and neuropsychiatric disturbances, including confusion and muscle weakness. In contrast to hypocalcemia, which primarily causes neuromuscular irritability, hypercalcemia poses a significant threat to cardiovascular and renal health.
Complications of Hypocalcemia
Hypocalcemia can lead to severe complications such as muscle spasms, tetany, and cardiac arrhythmias due to low calcium levels disrupting neuromuscular and cardiac function. Chronic hypocalcemia may cause neurological symptoms including seizures and cognitive impairment, increasing risks of long-term morbidity. Prompt diagnosis and calcium supplementation are critical to prevent life-threatening complications in patients with hypocalcemia.
Treatment and Management Approaches
Hypercalcemia treatment often involves intravenous hydration with saline and bisphosphonates to reduce serum calcium levels, while severe cases may require dialysis. Hypocalcemia management typically includes calcium supplementation, either orally or intravenously, alongside vitamin D analogs to enhance calcium absorption. Regular monitoring of serum calcium and underlying causes is essential to tailor treatment and prevent complications.
Prevention and Monitoring
Consistent monitoring of serum calcium levels is crucial for preventing hypercalcemia and hypocalcemia, with regular blood tests enabling early detection and management. Maintaining a balanced diet rich in calcium and vitamin D, along with appropriate supplementation guided by healthcare providers, helps regulate calcium homeostasis. Routine evaluation of parathyroid hormone (PTH) and kidney function further supports the prevention of calcium imbalance-related complications.
Hypercalcemia vs Hypocalcemia Infographic
 difterm.com
difterm.com