Oligomenorrhea refers to infrequent or irregular menstrual cycles lasting more than 35 days, while amenorrhea is the complete absence of menstruation for three or more months. Both conditions can be caused by hormonal imbalances, stress, or underlying medical issues such as polycystic ovary syndrome (PCOS) and thyroid disorders. Accurate diagnosis and targeted treatment are essential to restore normal menstrual function and address potential fertility concerns.
Table of Comparison
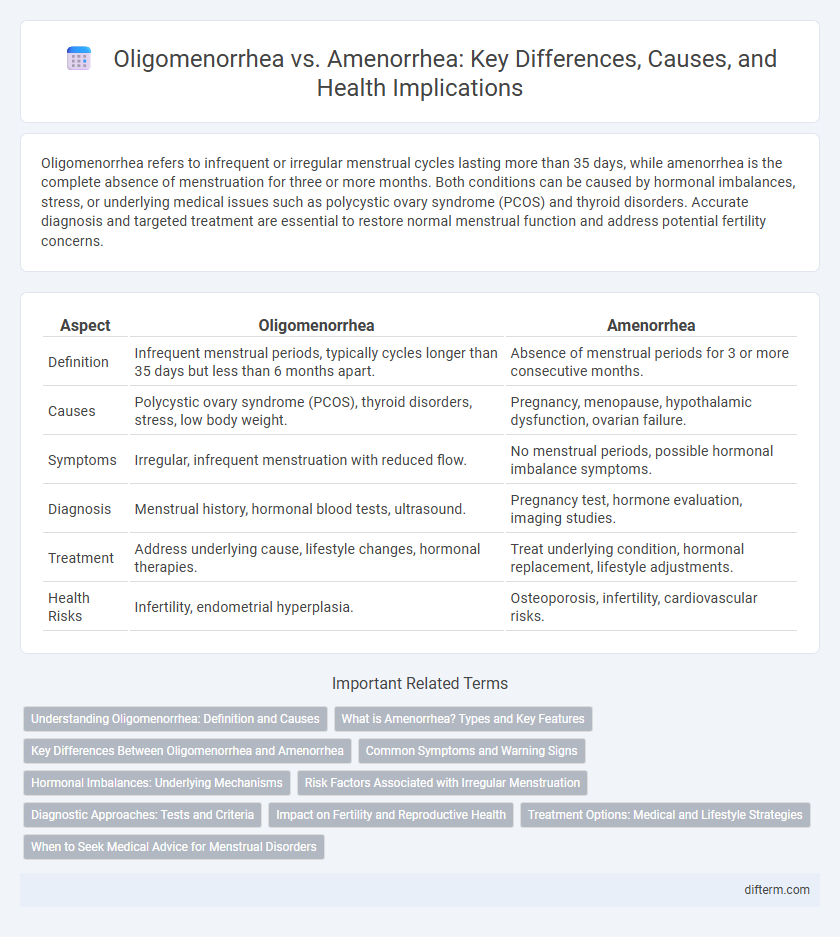
| Aspect | Oligomenorrhea | Amenorrhea |
|---|---|---|
| Definition | Infrequent menstrual periods, typically cycles longer than 35 days but less than 6 months apart. | Absence of menstrual periods for 3 or more consecutive months. |
| Causes | Polycystic ovary syndrome (PCOS), thyroid disorders, stress, low body weight. | Pregnancy, menopause, hypothalamic dysfunction, ovarian failure. |
| Symptoms | Irregular, infrequent menstruation with reduced flow. | No menstrual periods, possible hormonal imbalance symptoms. |
| Diagnosis | Menstrual history, hormonal blood tests, ultrasound. | Pregnancy test, hormone evaluation, imaging studies. |
| Treatment | Address underlying cause, lifestyle changes, hormonal therapies. | Treat underlying condition, hormonal replacement, lifestyle adjustments. |
| Health Risks | Infertility, endometrial hyperplasia. | Osteoporosis, infertility, cardiovascular risks. |
Understanding Oligomenorrhea: Definition and Causes
Oligomenorrhea refers to infrequent or irregular menstrual periods, typically defined as cycles longer than 35 days but less than 90 days, distinguishing it from amenorrhea, which is the complete absence of menstruation for three or more months. Common causes of oligomenorrhea include hormonal imbalances such as polycystic ovary syndrome (PCOS), thyroid dysfunction, and stress-related hypothalamic amenorrhea. Accurate diagnosis requires evaluating gynecological history, hormonal levels, and lifestyle factors to differentiate from other menstrual disorders.
What is Amenorrhea? Types and Key Features
Amenorrhea is the absence of menstruation, classified into primary and secondary types; primary amenorrhea refers to no menstruation by age 15, while secondary amenorrhea occurs when periods stop for three months or longer in previously menstruating women. Key features include hormonal imbalances, structural abnormalities, or underlying health conditions like polycystic ovary syndrome (PCOS) or thyroid disorders. Diagnosis often involves pelvic exams, hormone tests, and imaging to determine the cause and guide treatment.
Key Differences Between Oligomenorrhea and Amenorrhea
Oligomenorrhea is characterized by infrequent menstrual cycles, typically occurring more than 35 days apart, while amenorrhea involves the complete absence of menstruation for three months or more. Oligomenorrhea often indicates hormonal imbalances such as polycystic ovary syndrome (PCOS), whereas amenorrhea may signal more severe causes including pregnancy, hypothalamic dysfunction, or ovarian failure. Diagnosing the precise condition requires hormonal assessments, ultrasound imaging, and evaluation of underlying health issues to guide appropriate treatment.
Common Symptoms and Warning Signs
Oligomenorrhea is characterized by infrequent menstrual periods occurring more than 35 days apart, often accompanied by lighter bleeding, while amenorrhea involves the complete absence of menstruation for three or more consecutive months. Common symptoms of both conditions include irregular or missing periods, pelvic pain, and possible hormonal imbalances causing acne or excessive hair growth. Warning signs such as sudden onset, severe pelvic pain, or symptoms of underlying conditions like polycystic ovary syndrome (PCOS) or thyroid dysfunction require prompt medical evaluation.
Hormonal Imbalances: Underlying Mechanisms
Oligomenorrhea and amenorrhea both result from hormonal imbalances primarily involving disruptions in the hypothalamic-pituitary-ovarian axis, leading to irregular or absent menstrual cycles. Reduced secretion of gonadotropin-releasing hormone (GnRH) alters luteinizing hormone (LH) and follicle-stimulating hormone (FSH) levels, impacting estrogen and progesterone production essential for normal menstruation. Conditions such as polycystic ovary syndrome (PCOS), thyroid dysfunction, and hyperprolactinemia frequently contribute to these underlying endocrine disturbances.
Risk Factors Associated with Irregular Menstruation
Oligomenorrhea and amenorrhea are menstrual disorders characterized by infrequent and absent periods, respectively, often linked to hormonal imbalances such as polycystic ovary syndrome (PCOS) and thyroid dysfunction. Risk factors for irregular menstruation include excessive physical stress, significant weight fluctuations, and chronic illnesses like diabetes and eating disorders that disrupt endocrine function. Identifying these factors is critical for diagnosis and treatment to prevent complications like infertility and bone density loss.
Diagnostic Approaches: Tests and Criteria
Oligomenorrhea and amenorrhea require distinct diagnostic approaches, with oligomenorrhea characterized by menstrual cycles longer than 35 days but less than six months apart, while amenorrhea involves the absence of menstruation for three consecutive cycles or six months. Key diagnostic tests include serum hormone evaluations such as follicle-stimulating hormone (FSH), luteinizing hormone (LH), prolactin, thyroid-stimulating hormone (TSH), and estradiol levels to identify endocrine disorders. Imaging studies like pelvic ultrasound are critical for assessing ovarian morphology and excluding structural abnormalities contributing to menstrual irregularities.
Impact on Fertility and Reproductive Health
Oligomenorrhea, characterized by infrequent menstrual cycles, often signals hormonal imbalances that can disrupt ovulation, thereby reducing fertility potential. Amenorrhea, the complete absence of menstruation, indicates a more severe reproductive dysfunction frequently linked to underlying conditions such as polycystic ovary syndrome (PCOS) or hypothalamic amenorrhea, significantly impairing fertility. Both disorders require medical evaluation to address reproductive health risks and enhance chances of conception.
Treatment Options: Medical and Lifestyle Strategies
Treatment options for oligomenorrhea and amenorrhea include hormonal therapies such as oral contraceptives or progesterone to regulate menstrual cycles and address underlying hormonal imbalances. Lifestyle modifications involving stress management, balanced nutrition, and regular exercise are crucial in restoring normal menstruation, especially when related to conditions like polycystic ovary syndrome (PCOS) or hypothalamic amenorrhea. In some cases, addressing thyroid disorders or hyperprolactinemia through targeted medications may be necessary to achieve menstrual regularity.
When to Seek Medical Advice for Menstrual Disorders
Women experiencing oligomenorrhea, characterized by infrequent menstrual cycles occurring more than 35 days apart, or amenorrhea, defined as the complete absence of menstruation for three months or more, should seek medical advice to evaluate underlying causes such as hormonal imbalances, polycystic ovary syndrome (PCOS), or thyroid dysfunction. Immediate consultation is crucial if menstrual irregularities are accompanied by symptoms like severe pelvic pain, excessive hair growth, sudden weight changes, or signs of pregnancy. Early diagnosis and treatment of these menstrual disorders can prevent complications related to fertility, bone density, and cardiovascular health.
Oligomenorrhea vs amenorrhea Infographic
 difterm.com
difterm.com