Celiac disease is an autoimmune disorder where ingestion of gluten damages the small intestine, leading to severe nutrient absorption issues. Gluten sensitivity, or non-celiac gluten sensitivity, causes symptoms similar to celiac but without intestinal damage or autoimmune response. Proper diagnosis is essential to differentiate between the two conditions and implement an effective gluten-free diet for symptom management.
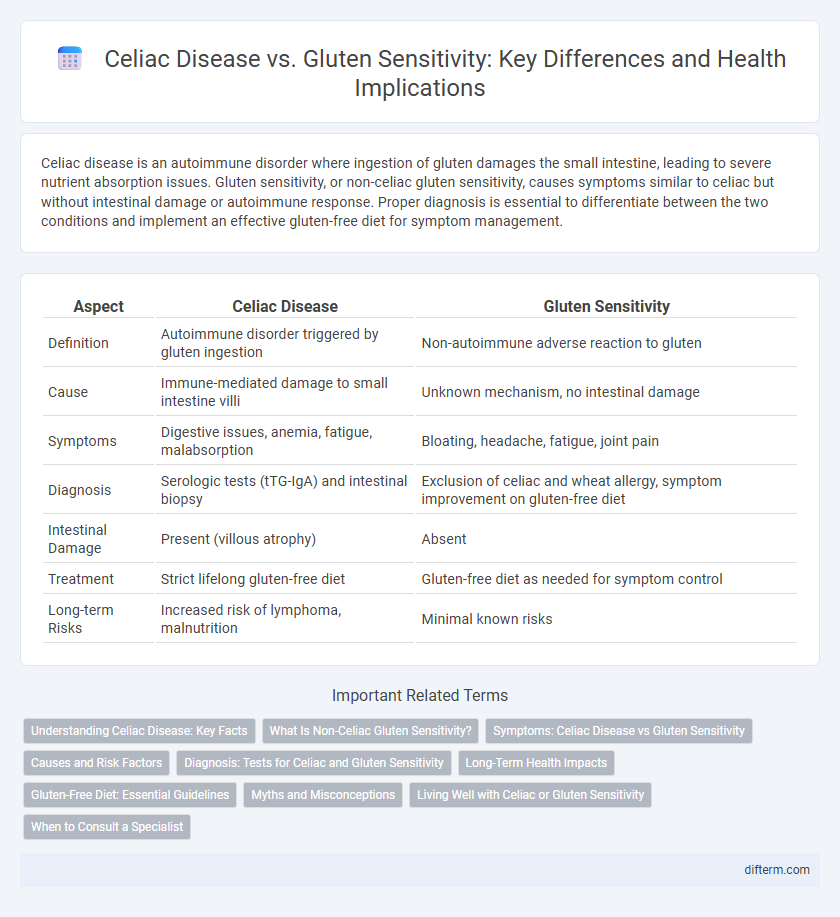
Table of Comparison
| Aspect | Celiac Disease | Gluten Sensitivity |
|---|---|---|
| Definition | Autoimmune disorder triggered by gluten ingestion | Non-autoimmune adverse reaction to gluten |
| Cause | Immune-mediated damage to small intestine villi | Unknown mechanism, no intestinal damage |
| Symptoms | Digestive issues, anemia, fatigue, malabsorption | Bloating, headache, fatigue, joint pain |
| Diagnosis | Serologic tests (tTG-IgA) and intestinal biopsy | Exclusion of celiac and wheat allergy, symptom improvement on gluten-free diet |
| Intestinal Damage | Present (villous atrophy) | Absent |
| Treatment | Strict lifelong gluten-free diet | Gluten-free diet as needed for symptom control |
| Long-term Risks | Increased risk of lymphoma, malnutrition | Minimal known risks |
Understanding Celiac Disease: Key Facts
Celiac disease is an autoimmune disorder triggered by gluten, a protein found in wheat, barley, and rye, leading to damage in the small intestine. Key symptoms include diarrhea, bloating, fatigue, and nutrient malabsorption, which can cause long-term health complications if untreated. Diagnosis requires specific blood tests and intestinal biopsy, differentiating it from non-celiac gluten sensitivity, which lacks the autoimmune component and intestinal damage.
What Is Non-Celiac Gluten Sensitivity?
Non-Celiac Gluten Sensitivity (NCGS) is a condition characterized by adverse reactions to gluten ingestion without the autoimmune response or intestinal damage seen in celiac disease. Symptoms include abdominal pain, bloating, diarrhea, headache, and fatigue, occurring shortly after gluten consumption and improving with a gluten-free diet. Diagnosing NCGS involves ruling out celiac disease and wheat allergy through specific blood tests and biopsies, making clinical assessment crucial for management.
Symptoms: Celiac Disease vs Gluten Sensitivity
Celiac disease symptoms include severe abdominal pain, diarrhea, weight loss, and nutrient deficiencies due to intestinal damage, while gluten sensitivity typically causes milder manifestations like bloating, fatigue, and headaches without intestinal injury. Both conditions may present overlapping gastrointestinal complaints, but celiac disease requires strict gluten avoidance to prevent long-term complications such as osteoporosis and neurological disorders. Accurate diagnosis through serologic testing and biopsy distinguishes celiac disease from gluten sensitivity, guiding appropriate treatment and dietary management.
Causes and Risk Factors
Celiac disease is an autoimmune disorder triggered by consuming gluten, a protein found in wheat, barley, and rye, causing damage to the small intestine's lining. Gluten sensitivity, also known as non-celiac gluten sensitivity, involves adverse reactions to gluten without intestinal damage or autoimmune markers. Genetic predisposition, including HLA-DQ2 and HLA-DQ8 genes, significantly increases the risk of celiac disease, while gluten sensitivity risk factors are less defined but may involve immune system responses and gut microbiota imbalances.
Diagnosis: Tests for Celiac and Gluten Sensitivity
Diagnosis of celiac disease involves serological tests such as tissue transglutaminase antibodies (tTG-IgA) and endomysial antibodies (EMA), followed by a confirmatory intestinal biopsy to assess villous atrophy. Gluten sensitivity lacks specific biomarkers, making diagnosis reliant on clinical assessment, symptom evaluation, and exclusion of celiac disease and wheat allergy through negative serology and biopsy. Accurate differentiation is critical for effective dietary management and prevention of complications.
Long-Term Health Impacts
Celiac disease causes autoimmune damage to the small intestine, leading to nutrient malabsorption, increased risk of osteoporosis, and higher chances of developing other autoimmune disorders if untreated over the long term. Non-celiac gluten sensitivity involves symptoms like gastrointestinal discomfort and fatigue without intestinal damage, generally not associated with serious long-term complications. Strict gluten avoidance is critical for celiac patients to prevent chronic health issues, while gluten-sensitive individuals may manage symptoms with less strict dietary measures.
Gluten-Free Diet: Essential Guidelines
Adopting a gluten-free diet is crucial for managing both celiac disease and gluten sensitivity, requiring strict avoidance of wheat, barley, and rye to prevent adverse immune reactions and intestinal damage. Emphasis on naturally gluten-free foods such as fruits, vegetables, lean proteins, and gluten-free grains like quinoa and rice ensures balanced nutrition and symptom relief. Reading food labels carefully and avoiding cross-contamination are essential steps to maintain a safe gluten-free lifestyle and improve long-term health outcomes.
Myths and Misconceptions
Celiac disease is an autoimmune disorder triggered by gluten ingestion, while gluten sensitivity causes similar symptoms without autoimmune damage, but misunderstandings often conflate the two conditions. A common myth is that gluten sensitivity is a milder form of celiac disease, ignoring distinct immune responses and diagnostic criteria. Many believe gluten-free diets benefit all digestive issues, yet evidence supports this only for celiac disease and proven gluten sensitivity, not general digestive problems.
Living Well with Celiac or Gluten Sensitivity
Managing celiac disease requires strict adherence to a gluten-free diet to prevent intestinal damage and related complications, while those with gluten sensitivity often experience symptom relief by avoiding gluten without the risk of long-term gut harm. Incorporating naturally gluten-free foods like fruits, vegetables, lean proteins, and gluten-free grains supports nutritional balance and overall well-being. Regular medical check-ups and consultations with dietitians specializing in gluten-related disorders enhance symptom management and improve quality of life for individuals living with either condition.
When to Consult a Specialist
Persistent digestive symptoms such as chronic diarrhea, abdominal pain, or unexplained weight loss warrant consultation with a gastroenterologist to differentiate between celiac disease and non-celiac gluten sensitivity. Blood tests measuring tissue transglutaminase antibodies (tTG-IgA) and endomysial antibodies (EMA) help confirm celiac disease, while gluten sensitivity diagnosis relies on symptom assessment and exclusion of other conditions. Early specialist evaluation prevents complications like intestinal damage, ensuring appropriate dietary management for long-term gastrointestinal health.
Celiac vs Gluten Sensitivity Infographic
 difterm.com
difterm.com