Cholangitis is an infection of the bile ducts often caused by obstruction or gallstones, leading to symptoms like fever, jaundice, and abdominal pain. Cholecystitis refers to inflammation of the gallbladder, typically resulting from gallstone obstruction, causing intense right upper quadrant pain and tenderness. Accurate diagnosis through imaging and lab tests is crucial for differentiating between these conditions and guiding appropriate treatment.
Table of Comparison
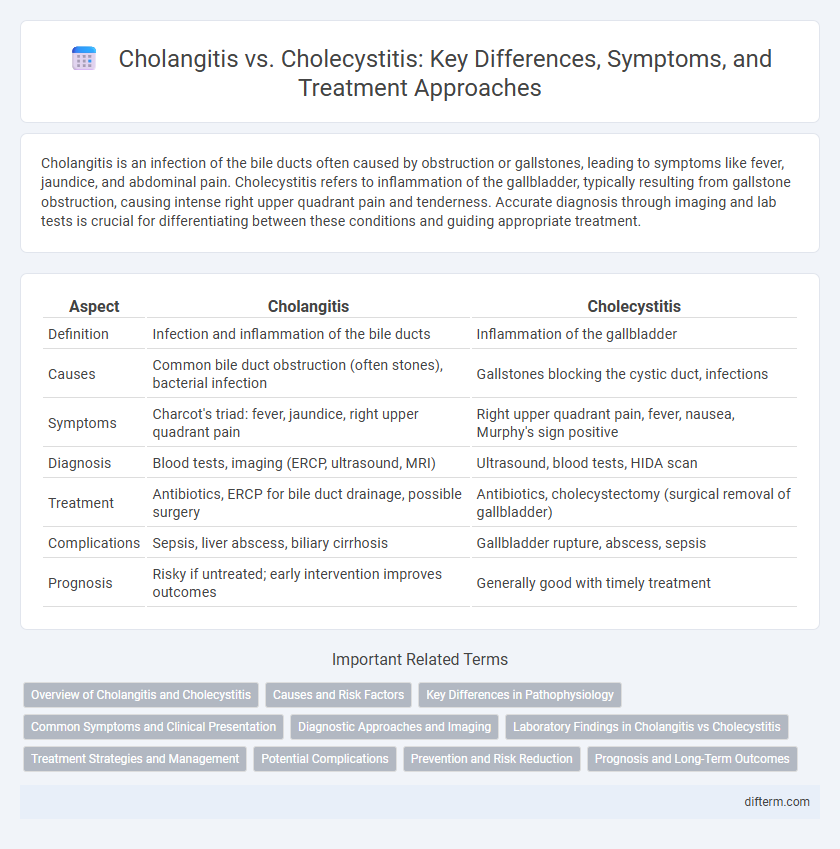
| Aspect | Cholangitis | Cholecystitis |
|---|---|---|
| Definition | Infection and inflammation of the bile ducts | Inflammation of the gallbladder |
| Causes | Common bile duct obstruction (often stones), bacterial infection | Gallstones blocking the cystic duct, infections |
| Symptoms | Charcot's triad: fever, jaundice, right upper quadrant pain | Right upper quadrant pain, fever, nausea, Murphy's sign positive |
| Diagnosis | Blood tests, imaging (ERCP, ultrasound, MRI) | Ultrasound, blood tests, HIDA scan |
| Treatment | Antibiotics, ERCP for bile duct drainage, possible surgery | Antibiotics, cholecystectomy (surgical removal of gallbladder) |
| Complications | Sepsis, liver abscess, biliary cirrhosis | Gallbladder rupture, abscess, sepsis |
| Prognosis | Risky if untreated; early intervention improves outcomes | Generally good with timely treatment |
Overview of Cholangitis and Cholecystitis
Cholangitis is an infection of the bile ducts often caused by bacterial obstruction, leading to symptoms such as jaundice, fever, and abdominal pain. Cholecystitis involves inflammation of the gallbladder, typically due to gallstones blocking the cystic duct, presenting with right upper quadrant pain and tenderness. Both conditions require prompt medical evaluation but differ in their anatomical focus and underlying causes.
Causes and Risk Factors
Cholangitis is primarily caused by bacterial infection due to bile duct obstruction often linked to gallstones, strictures, or tumors, with risk factors including advanced age, bile duct procedures, and immune-compromised conditions. Cholecystitis arises mainly from gallstone obstruction of the cystic duct, leading to inflammation of the gallbladder, with risk factors such as female gender, obesity, pregnancy, and rapid weight loss. Both conditions involve bile flow disruption but differ in anatomical focus and predisposing elements impacting their development.
Key Differences in Pathophysiology
Cholangitis involves infection and inflammation of the bile ducts, often caused by bacterial invasion due to bile duct obstruction, leading to bile stasis and potential sepsis. Cholecystitis is characterized by inflammation of the gallbladder, typically resulting from gallstone impaction in the cystic duct, causing gallbladder wall ischemia and local inflammation. The key pathophysiological difference lies in cholangitis affecting the biliary tree with systemic infection risk, whereas cholecystitis primarily concerns localized gallbladder inflammation without initial ductal infection.
Common Symptoms and Clinical Presentation
Cholangitis typically presents with Charcot's triad: fever, right upper quadrant abdominal pain, and jaundice, often accompanied by chills and dark urine. Cholecystitis manifests with constant right upper quadrant pain, fever, nausea, vomiting, and a positive Murphy's sign on physical examination. Both conditions involve inflammation of the biliary system but differ in symptom onset and clinical severity, guiding diagnostic and therapeutic approaches.
Diagnostic Approaches and Imaging
Cholangitis diagnosis primarily relies on blood tests showing elevated liver enzymes and bilirubin, alongside imaging techniques like ultrasound, Magnetic Resonance Cholangiopancreatography (MRCP), or Endoscopic Retrograde Cholangiopancreatography (ERCP) to detect bile duct obstruction and inflammation. Cholecystitis is usually diagnosed through ultrasound revealing gallbladder wall thickening, pericholecystic fluid, and gallstones, with hepatobiliary iminodiacetic acid (HIDA) scan used to assess gallbladder function in ambiguous cases. Cross-sectional imaging such as computed tomography (CT) also aids in distinguishing complications between both conditions.
Laboratory Findings in Cholangitis vs Cholecystitis
Laboratory findings in cholangitis typically reveal elevated alkaline phosphatase, gamma-glutamyl transferase, bilirubin, and leukocytosis, indicating bile duct obstruction and infection. In contrast, cholecystitis often presents with increased white blood cell count, mild elevations in liver enzymes, and normal or slightly elevated bilirubin levels, reflecting localized gallbladder inflammation without major bile duct involvement. Blood cultures in cholangitis may be positive due to systemic infection, whereas cholecystitis rarely shows bacteremia.
Treatment Strategies and Management
Cholangitis treatment prioritizes urgent antibiotic therapy combined with biliary drainage techniques such as endoscopic retrograde cholangiopancreatography (ERCP) to relieve biliary obstruction. Cholecystitis management often involves pain control, antibiotics targeting common pathogens like E. coli and Klebsiella, and laparoscopic cholecystectomy as a definitive surgical intervention. Prompt differentiation and tailored approaches reduce complications and improve patient outcomes in both conditions.
Potential Complications
Cholangitis potential complications include sepsis, liver abscess, and biliary cirrhosis due to infection and bile duct obstruction. In contrast, cholecystitis complications may involve gallbladder perforation, empyema, and gangrene resulting from inflammation and ischemia of the gallbladder wall. Both conditions require prompt diagnosis and treatment to prevent severe morbidity and mortality.
Prevention and Risk Reduction
Cholangitis prevention centers on maintaining bile duct health through timely treatment of gallstones and strict hygiene during invasive procedures like ERCP to reduce bacterial infections. Reducing cholecystitis risk involves a low-fat diet, regular exercise to prevent gallstone formation, and managing conditions like obesity and diabetes. Early diagnosis and managing underlying conditions significantly decrease complications related to both cholangitis and cholecystitis.
Prognosis and Long-Term Outcomes
Cholangitis prognosis depends on timely antibiotic treatment and biliary drainage, with delayed intervention increasing the risk of sepsis and liver abscesses, potentially leading to chronic biliary strictures. Cholecystitis typically has a favorable long-term outcome after cholecystectomy, although complications like gallbladder rupture or bile peritonitis can worsen prognosis. Both conditions require early diagnosis to prevent chronic complications, but cholangitis generally carries a higher risk of severe systemic effects and recurrence.
Cholangitis vs Cholecystitis Infographic
 difterm.com
difterm.com