Autoimmunity occurs when the immune system mistakenly attacks the body's own tissues, leading to chronic inflammation and tissue damage. Allergy involves an overreaction of the immune system to harmless substances like pollen or food, causing symptoms such as itching, swelling, or respiratory distress. Understanding the differences between autoimmunity and allergy is crucial for accurate diagnosis and effective treatment strategies.
Table of Comparison
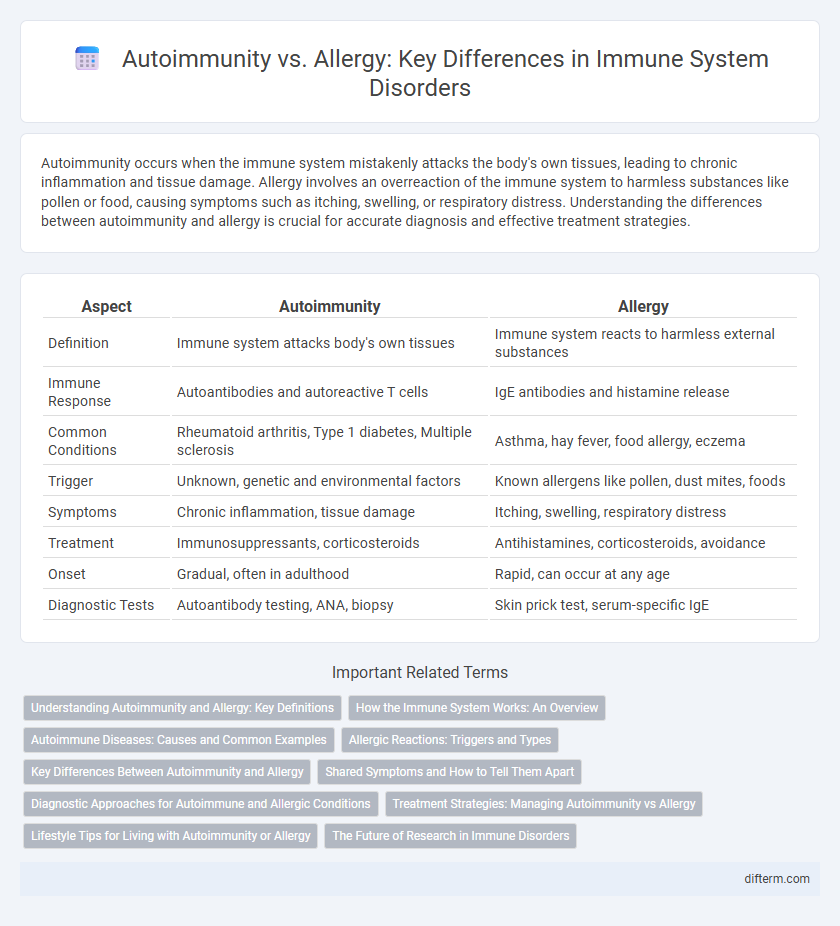
| Aspect | Autoimmunity | Allergy |
|---|---|---|
| Definition | Immune system attacks body's own tissues | Immune system reacts to harmless external substances |
| Immune Response | Autoantibodies and autoreactive T cells | IgE antibodies and histamine release |
| Common Conditions | Rheumatoid arthritis, Type 1 diabetes, Multiple sclerosis | Asthma, hay fever, food allergy, eczema |
| Trigger | Unknown, genetic and environmental factors | Known allergens like pollen, dust mites, foods |
| Symptoms | Chronic inflammation, tissue damage | Itching, swelling, respiratory distress |
| Treatment | Immunosuppressants, corticosteroids | Antihistamines, corticosteroids, avoidance |
| Onset | Gradual, often in adulthood | Rapid, can occur at any age |
| Diagnostic Tests | Autoantibody testing, ANA, biopsy | Skin prick test, serum-specific IgE |
Understanding Autoimmunity and Allergy: Key Definitions
Autoimmunity is a condition where the immune system mistakenly attacks the body's own tissues, leading to diseases such as rheumatoid arthritis and lupus. Allergy refers to an exaggerated immune response to external substances like pollen, food, or pet dander, causing symptoms including itching, swelling, and anaphylaxis. Differentiating autoimmunity from allergy is essential for accurate diagnosis and targeted treatment strategies in immunological disorders.
How the Immune System Works: An Overview
The immune system defends the body by recognizing and responding to harmful substances, distinguishing between self and non-self. In autoimmunity, the immune system mistakenly targets the body's own tissues, causing chronic inflammation and tissue damage. Allergies occur when the immune system overreacts to harmless external substances, triggering symptoms like swelling, itching, or respiratory issues.
Autoimmune Diseases: Causes and Common Examples
Autoimmune diseases occur when the immune system mistakenly attacks the body's own tissues, triggered by genetic predisposition, environmental factors, and infections. Common examples include rheumatoid arthritis, lupus erythematosus, and type 1 diabetes, each characterized by chronic inflammation and tissue damage. Understanding these causes helps differentiate autoimmune responses from allergies, which involve hypersensitive reactions to external allergens.
Allergic Reactions: Triggers and Types
Allergic reactions occur when the immune system overreacts to harmless substances known as allergens, such as pollen, pet dander, or certain foods. These reactions can be classified into four main types: Type I (immediate hypersensitivity), Type II (cytotoxic), Type III (immune complex-mediated), and Type IV (delayed-type hypersensitivity). Common triggers include environmental factors, insect stings, medications, and food proteins, leading to symptoms ranging from mild rashes to severe anaphylaxis.
Key Differences Between Autoimmunity and Allergy
Autoimmunity involves the immune system mistakenly attacking the body's own tissues, leading to chronic inflammation and tissue damage, whereas allergy is an exaggerated immune response to external allergens like pollen or food proteins. Autoimmune diseases, such as rheumatoid arthritis and multiple sclerosis, result from immune dysregulation targeting self-antigens, while allergic reactions, including hay fever and anaphylaxis, are mediated by IgE antibodies against harmless substances. The key difference lies in autoimmunity's self-directed immune attack versus allergy's hypersensitivity to environmental triggers.
Shared Symptoms and How to Tell Them Apart
Autoimmunity and allergy share common symptoms such as inflammation, fatigue, and skin rashes, making initial diagnosis challenging. Autoimmune diseases like lupus and rheumatoid arthritis involve the immune system attacking the body's own tissues, whereas allergies trigger immune responses to external substances like pollen or food allergens. Differentiation relies on specific diagnostic tests including antibody panels for autoimmune markers and skin or blood tests for allergen sensitivity.
Diagnostic Approaches for Autoimmune and Allergic Conditions
Diagnostic approaches for autoimmune conditions primarily involve autoantibody testing, such as antinuclear antibodies (ANA) and rheumatoid factor (RF), alongside inflammatory markers like ESR and CRP. Allergy diagnostics focus on skin prick tests, specific IgE blood tests, and elimination diets to identify allergens triggering hypersensitivity reactions. Advanced techniques like flow cytometry and molecular assays enhance the accuracy of differentiating autoimmune disorders from allergic responses.
Treatment Strategies: Managing Autoimmunity vs Allergy
Treatment strategies for autoimmunity focus on immune system suppression using corticosteroids, immunosuppressants, and biologics to reduce self-reactive immune responses. Allergy management primarily involves avoiding allergens, antihistamines, corticosteroids, and immunotherapy to desensitize the immune system to specific triggers. Personalized treatment plans are essential to effectively control symptoms and improve quality of life in both autoimmune diseases and allergic conditions.
Lifestyle Tips for Living with Autoimmunity or Allergy
Managing autoimmunity or allergies involves adopting lifestyle habits such as maintaining a balanced diet rich in anti-inflammatory foods, ensuring regular physical activity, and minimizing exposure to known triggers. Prioritizing stress reduction techniques like mindfulness or yoga can help regulate immune response and improve overall well-being. Consistent sleep patterns and regular medical check-ups play a critical role in monitoring symptoms and preventing flare-ups.
The Future of Research in Immune Disorders
Emerging research in immune disorders is increasingly focusing on distinguishing the molecular pathways that differentiate autoimmunity from allergy to develop targeted therapies. Advances in genomics and proteomics are facilitating the identification of specific biomarkers for early diagnosis and personalized treatment approaches. Cutting-edge technologies such as CRISPR gene editing and biopharmaceutical innovations hold promise for modulating immune responses and potentially curing these chronic conditions.
Autoimmunity vs Allergy Infographic
 difterm.com
difterm.com