Acute kidney injury (AKI) is a sudden and reversible loss of kidney function often caused by dehydration, toxins, or infections, while chronic kidney disease (CKD) involves gradual, irreversible damage leading to long-term kidney failure. Early detection of AKI allows for immediate treatment to prevent permanent damage, whereas CKD management focuses on slowing progression through diet, medication, and monitoring. Recognizing the differences between AKI and CKD is crucial for effective veterinary care and improving pets' quality of life.
Table of Comparison
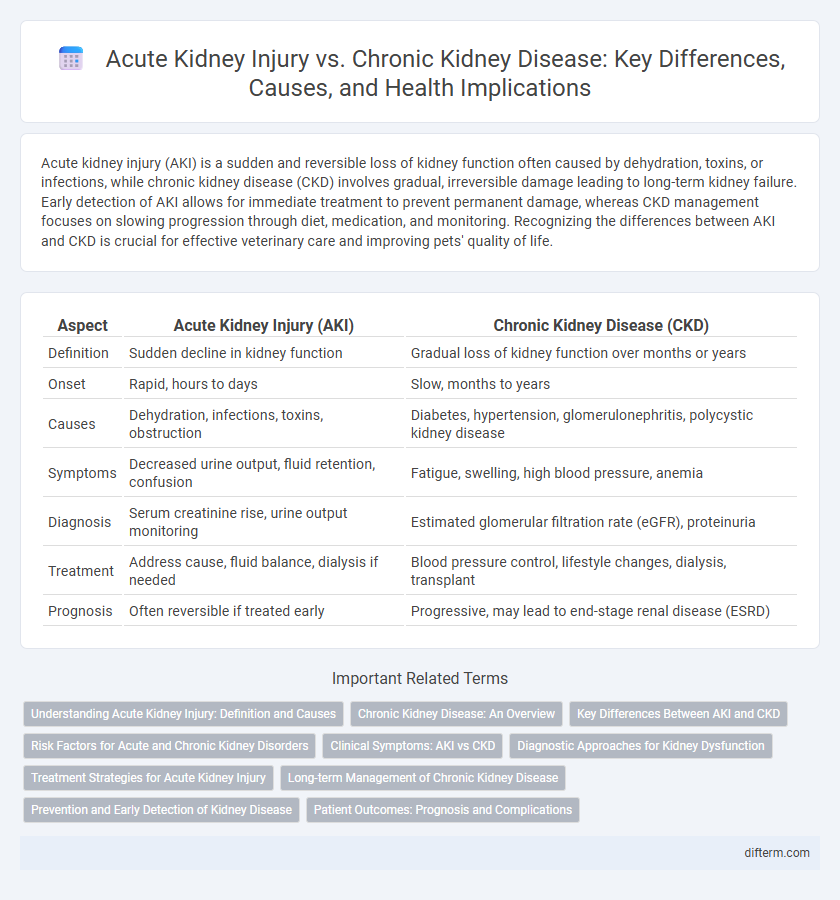
| Aspect | Acute Kidney Injury (AKI) | Chronic Kidney Disease (CKD) |
|---|---|---|
| Definition | Sudden decline in kidney function | Gradual loss of kidney function over months or years |
| Onset | Rapid, hours to days | Slow, months to years |
| Causes | Dehydration, infections, toxins, obstruction | Diabetes, hypertension, glomerulonephritis, polycystic kidney disease |
| Symptoms | Decreased urine output, fluid retention, confusion | Fatigue, swelling, high blood pressure, anemia |
| Diagnosis | Serum creatinine rise, urine output monitoring | Estimated glomerular filtration rate (eGFR), proteinuria |
| Treatment | Address cause, fluid balance, dialysis if needed | Blood pressure control, lifestyle changes, dialysis, transplant |
| Prognosis | Often reversible if treated early | Progressive, may lead to end-stage renal disease (ESRD) |
Understanding Acute Kidney Injury: Definition and Causes
Acute kidney injury (AKI) is a sudden decline in kidney function, characterized by an abrupt reduction in glomerular filtration rate, often caused by conditions such as sepsis, dehydration, or nephrotoxic drugs. Unlike chronic kidney disease (CKD), which progresses slowly over months to years, AKI develops rapidly and may be reversible with prompt diagnosis and treatment. Early identification of AKI through biomarkers like serum creatinine and urine output is crucial to prevent permanent kidney damage and transition to chronic disease.
Chronic Kidney Disease: An Overview
Chronic Kidney Disease (CKD) is a progressive condition characterized by the gradual loss of kidney function over time, often caused by diabetes, hypertension, and glomerulonephritis. Unlike Acute Kidney Injury (AKI), which involves sudden kidney damage, CKD leads to long-term complications such as cardiovascular disease, anemia, and bone disorders. Early detection through estimated glomerular filtration rate (eGFR) and urine albumin tests is crucial for managing CKD and slowing its progression.
Key Differences Between AKI and CKD
Acute kidney injury (AKI) is characterized by a sudden decline in kidney function, often reversible with timely intervention, whereas chronic kidney disease (CKD) involves gradual, irreversible loss of renal function over months or years. AKI typically presents with rapid elevation in serum creatinine and reduced urine output, while CKD is diagnosed by persistent abnormalities in kidney markers such as estimated glomerular filtration rate (eGFR) below 60 mL/min/1.73 m2 for over three months. Causes of AKI include acute events like sepsis or nephrotoxic drugs, contrasting with CKD's common etiologies such as diabetes mellitus and hypertension-induced nephropathy.
Risk Factors for Acute and Chronic Kidney Disorders
Risk factors for acute kidney injury (AKI) include dehydration, sepsis, exposure to nephrotoxic drugs, and major surgery, particularly cardiac and vascular procedures. Chronic kidney disease (CKD) is strongly associated with diabetes mellitus, hypertension, cardiovascular disease, and prolonged use of nephrotoxic medications. Early identification of these risk elements is crucial for preventing progression and improving patient outcomes in both acute and chronic kidney disorders.
Clinical Symptoms: AKI vs CKD
Acute kidney injury (AKI) manifests with abrupt symptoms such as decreased urine output, fluid retention, and confusion due to sudden loss of kidney function. Chronic kidney disease (CKD) often presents with gradual fatigue, swelling in extremities, and persistent high blood pressure as kidney damage progresses over months or years. Unlike AKI's rapid onset, CKD symptoms develop insidiously, leading to anemia, bone disease, and metabolic imbalances in advanced stages.
Diagnostic Approaches for Kidney Dysfunction
Acute kidney injury (AKI) diagnosis relies on rapid assessment of serum creatinine levels and urine output to detect sudden renal function decline, often supplemented by imaging studies such as renal ultrasound to rule out obstruction. Chronic kidney disease (CKD) diagnosis emphasizes persistent markers of kidney damage over three months, including estimated glomerular filtration rate (eGFR) reduction and albuminuria measurement through urine albumin-to-creatinine ratio (UACR). Biomarkers like cystatin C and novel urinary proteins are increasingly integrated to improve early detection and differentiate acute from chronic kidney impairments in clinical practice.
Treatment Strategies for Acute Kidney Injury
Treatment strategies for acute kidney injury (AKI) primarily focus on addressing the underlying cause, optimizing fluid balance, and preventing further kidney damage. Interventions may include fluid resuscitation, electrolyte management, and renal replacement therapy such as dialysis in severe cases. Early detection and prompt management are critical to improving patient outcomes and reducing the risk of progression to chronic kidney disease (CKD).
Long-term Management of Chronic Kidney Disease
Long-term management of chronic kidney disease (CKD) involves regular monitoring of glomerular filtration rate (GFR), blood pressure control, and minimizing proteinuria through angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs). Nutritional interventions emphasize low-protein diets and phosphorus restriction to slow disease progression and reduce complications. Early intervention in CKD reduces the risk of cardiovascular events and delays the need for renal replacement therapy such as dialysis or transplantation.
Prevention and Early Detection of Kidney Disease
Preventing acute kidney injury (AKI) and chronic kidney disease (CKD) involves controlling risk factors such as hypertension, diabetes, and dehydration while avoiding nephrotoxic drugs. Early detection relies on regular monitoring of serum creatinine, estimated glomerular filtration rate (eGFR), and urine albumin-to-creatinine ratio (ACR) in at-risk populations. Timely intervention through lifestyle modification and medical management reduces progression rates and improves kidney health outcomes.
Patient Outcomes: Prognosis and Complications
Acute kidney injury (AKI) often results in rapid loss of kidney function with potential for full recovery if promptly treated, but it significantly raises the risk of developing chronic kidney disease (CKD). Chronic kidney disease progresses gradually, leading to irreversible kidney damage, increased risk of cardiovascular events, and higher mortality rates. Patient outcomes in CKD are frequently complicated by hypertension, anemia, and electrolyte imbalances, necessitating continuous management to delay progression and improve quality of life.
Acute kidney injury vs Chronic kidney disease Infographic
 difterm.com
difterm.com