Bacterial vaginosis is characterized by an imbalance in the vaginal microbiota, leading to symptoms such as thin, grayish discharge with a fishy odor, whereas candidiasis is caused by an overgrowth of Candida yeast, resulting in thick, white, cottage cheese-like discharge and intense itching. Both conditions require accurate diagnosis through clinical examination and laboratory testing to ensure effective treatment. Antibiotics are commonly used for bacterial vaginosis, while antifungal medications target candidiasis.
Table of Comparison
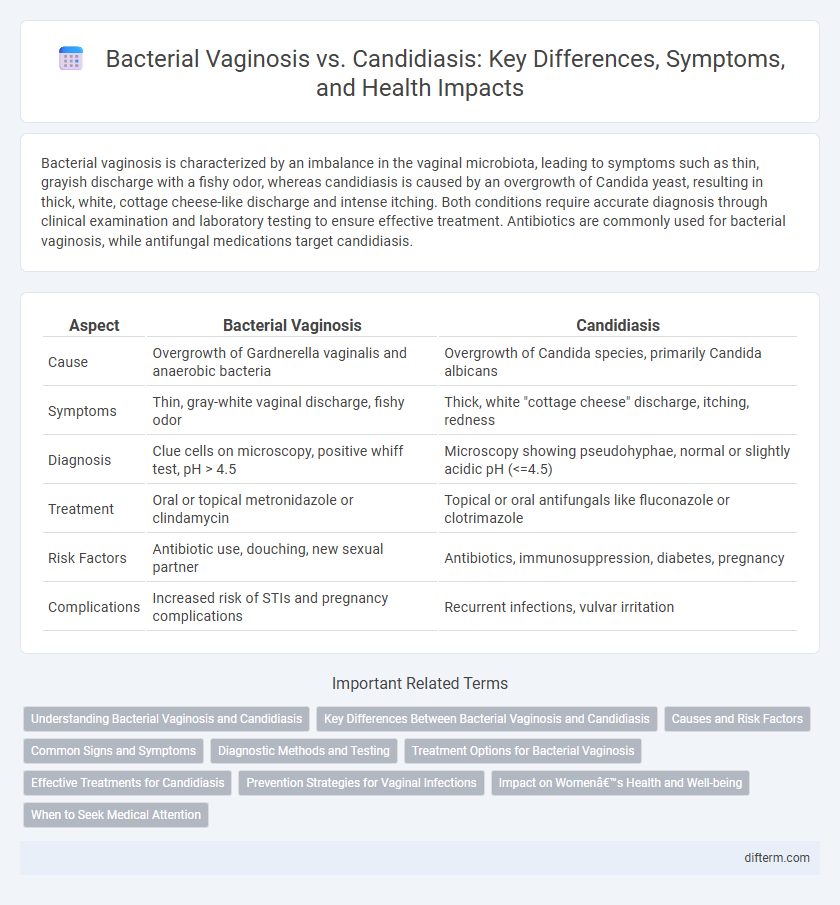
| Aspect | Bacterial Vaginosis | Candidiasis |
|---|---|---|
| Cause | Overgrowth of Gardnerella vaginalis and anaerobic bacteria | Overgrowth of Candida species, primarily Candida albicans |
| Symptoms | Thin, gray-white vaginal discharge, fishy odor | Thick, white "cottage cheese" discharge, itching, redness |
| Diagnosis | Clue cells on microscopy, positive whiff test, pH > 4.5 | Microscopy showing pseudohyphae, normal or slightly acidic pH (<=4.5) |
| Treatment | Oral or topical metronidazole or clindamycin | Topical or oral antifungals like fluconazole or clotrimazole |
| Risk Factors | Antibiotic use, douching, new sexual partner | Antibiotics, immunosuppression, diabetes, pregnancy |
| Complications | Increased risk of STIs and pregnancy complications | Recurrent infections, vulvar irritation |
Understanding Bacterial Vaginosis and Candidiasis
Bacterial vaginosis (BV) results from an imbalance in the vaginal microbiota, characterized by a reduction in Lactobacillus species and an overgrowth of anaerobic bacteria such as Gardnerella vaginalis. Candidiasis, commonly caused by Candida albicans, is a fungal infection leading to symptoms like itching, discharge, and inflammation. Differentiating between BV and candidiasis is critical for effective treatment, as BV responds to antibiotics while candidiasis requires antifungal therapy.
Key Differences Between Bacterial Vaginosis and Candidiasis
Bacterial vaginosis is characterized by an imbalance of the vaginal microbiota, primarily involving the overgrowth of Gardnerella vaginalis, resulting in a thin, grayish discharge with a fishy odor. Candidiasis, commonly caused by Candida albicans, leads to thick, white, cottage cheese-like discharge accompanied by itching and redness. Diagnosis often involves microscopic examination and pH testing, with bacterial vaginosis presenting a vaginal pH above 4.5, whereas candidiasis typically maintains a normal vaginal pH of 4.0 to 4.5.
Causes and Risk Factors
Bacterial vaginosis is primarily caused by an imbalance in the vaginal microbiota, with a reduction in Lactobacillus species and an overgrowth of anaerobic bacteria such as Gardnerella vaginalis. Candidiasis occurs due to the overgrowth of Candida species, especially Candida albicans, often triggered by antibiotic use, hormonal changes, or immunosuppression. Risk factors for bacterial vaginosis include multiple sexual partners and douching, while candidiasis risk factors involve diabetes, pregnancy, and prolonged corticosteroid therapy.
Common Signs and Symptoms
Bacterial vaginosis typically presents with a thin, grayish-white vaginal discharge accompanied by a fishy odor, especially after intercourse. In contrast, candidiasis (yeast infection) is characterized by thick, white, cottage cheese-like discharge and intense itching and redness of the vulva. Both conditions may cause discomfort and irritation, but their distinct symptoms help in accurate diagnosis and targeted treatment.
Diagnostic Methods and Testing
Bacterial vaginosis diagnosis involves microscopic examination of vaginal discharge, identifying clue cells, and assessing vaginal pH, which is typically above 4.5, alongside a positive whiff test for amines. In contrast, candidiasis diagnosis relies on direct microscopic visualization of yeast cells or pseudohyphae in a potassium hydroxide (KOH) preparation and fungal culture for species identification. Molecular testing such as nucleic acid amplification tests (NAATs) can enhance detection accuracy for both infections, differentiating between Gardnerella vaginalis in bacterial vaginosis and Candida species in candidiasis.
Treatment Options for Bacterial Vaginosis
Bacterial vaginosis treatment primarily involves antibiotic therapies such as metronidazole or clindamycin, which target the overgrowth of Gardnerella vaginalis and other anaerobic bacteria. Probiotic supplements containing Lactobacillus strains may help restore the natural vaginal flora but are considered adjunctive rather than standalone treatments. Avoiding douching and unprotected sexual activity can reduce recurrence rates and improve treatment efficacy.
Effective Treatments for Candidiasis
Effective treatments for candidiasis primarily include antifungal medications such as fluconazole and topical clotrimazole, which target Candida yeast infections. Maintaining proper vaginal pH balance and hygiene supports recovery and reduces recurrence risk. Unlike bacterial vaginosis, candidiasis responds specifically to antifungal therapy rather than antibiotics.
Prevention Strategies for Vaginal Infections
Maintaining proper vaginal hygiene by avoiding douching and using mild, unscented products helps prevent bacterial vaginosis and candidiasis by preserving the natural pH balance and microbiota. Wearing breathable, cotton underwear and avoiding tight-fitting clothing reduce moisture buildup, which lowers the risk of fungal infections like candidiasis. Regularly practicing safe sex and promptly treating antibiotic-associated imbalances are critical strategies in minimizing the recurrence of bacterial vaginosis.
Impact on Women’s Health and Well-being
Bacterial vaginosis (BV) and candidiasis significantly affect women's health and well-being by causing discomfort, abnormal discharge, and increased susceptibility to other infections. BV disrupts the natural vaginal flora, leading to a higher risk of pelvic inflammatory disease and adverse pregnancy outcomes, while candidiasis primarily results in intense itching and inflammation that impair daily activities. Both conditions can negatively influence emotional health due to recurrent symptoms and social stigma, highlighting the need for timely diagnosis and effective treatment.
When to Seek Medical Attention
Seek medical attention for bacterial vaginosis if experiencing persistent vaginal odor, abnormal discharge, or itching, especially when symptoms interfere with daily life or recur frequently. For candidiasis, consult a healthcare provider when intense itching, thick white discharge, or pain during urination or intercourse occurs, or if over-the-counter treatments fail to resolve symptoms within a week. Prompt diagnosis ensures appropriate treatment, reducing the risk of complications and recurrence.
Bacterial vaginosis vs Candidiasis Infographic
 difterm.com
difterm.com