Subclinical hypothyroidism is characterized by elevated thyroid-stimulating hormone (TSH) levels with normal free thyroxine (T4) concentrations, often presenting mild or no symptoms. Overt hypothyroidism involves significantly increased TSH levels accompanied by low circulating thyroid hormones, leading to pronounced clinical symptoms like fatigue, weight gain, and cold intolerance. Early diagnosis and management are crucial to prevent progression from subclinical to overt hypothyroidism and associated complications such as cardiovascular disease.
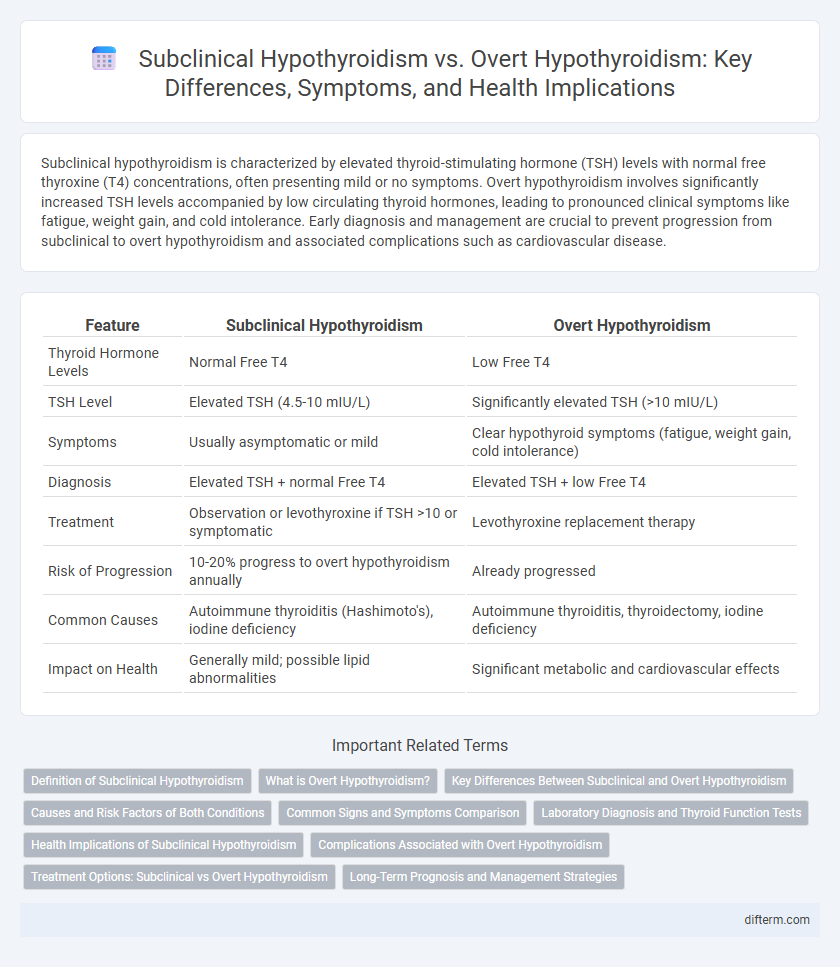
Table of Comparison
| Feature | Subclinical Hypothyroidism | Overt Hypothyroidism |
|---|---|---|
| Thyroid Hormone Levels | Normal Free T4 | Low Free T4 |
| TSH Level | Elevated TSH (4.5-10 mIU/L) | Significantly elevated TSH (>10 mIU/L) |
| Symptoms | Usually asymptomatic or mild | Clear hypothyroid symptoms (fatigue, weight gain, cold intolerance) |
| Diagnosis | Elevated TSH + normal Free T4 | Elevated TSH + low Free T4 |
| Treatment | Observation or levothyroxine if TSH >10 or symptomatic | Levothyroxine replacement therapy |
| Risk of Progression | 10-20% progress to overt hypothyroidism annually | Already progressed |
| Common Causes | Autoimmune thyroiditis (Hashimoto's), iodine deficiency | Autoimmune thyroiditis, thyroidectomy, iodine deficiency |
| Impact on Health | Generally mild; possible lipid abnormalities | Significant metabolic and cardiovascular effects |
Definition of Subclinical Hypothyroidism
Subclinical hypothyroidism is characterized by elevated serum thyroid-stimulating hormone (TSH) levels while maintaining normal free thyroxine (FT4) concentrations, indicating early or mild thyroid dysfunction without obvious clinical symptoms. Unlike overt hypothyroidism, which presents with low thyroid hormone levels and clear hypothyroid symptoms, subclinical hypothyroidism often requires careful monitoring to assess progression risk. Prevalence varies between 4% and 10% in the general population, with higher rates in women and older adults.
What is Overt Hypothyroidism?
Overt hypothyroidism is a clinical condition characterized by elevated thyroid-stimulating hormone (TSH) levels and decreased free thyroxine (T4) levels, leading to clear symptoms such as fatigue, weight gain, cold intolerance, and bradycardia. Unlike subclinical hypothyroidism, where thyroid hormone levels remain normal despite elevated TSH, overt hypothyroidism reflects significant thyroid hormone deficiency requiring immediate medical intervention. Diagnosis often involves serum TSH and free T4 testing, and treatment primarily consists of levothyroxine replacement therapy to restore normal metabolic function.
Key Differences Between Subclinical and Overt Hypothyroidism
Subclinical hypothyroidism is characterized by elevated thyroid-stimulating hormone (TSH) levels with normal free thyroxine (T4) levels, whereas overt hypothyroidism presents with both elevated TSH and low free T4 levels. Symptoms in subclinical hypothyroidism are often mild or absent, while overt hypothyroidism causes more pronounced clinical manifestations such as fatigue, weight gain, and cold intolerance. Diagnosis and treatment strategies differ, with subclinical hypothyroidism sometimes requiring monitoring without immediate therapy, whereas overt hypothyroidism typically necessitates thyroid hormone replacement.
Causes and Risk Factors of Both Conditions
Subclinical hypothyroidism is primarily caused by mild thyroid gland dysfunction, often due to autoimmune thyroiditis such as Hashimoto's disease, while overt hypothyroidism results from more severe thyroid hormone deficiency commonly linked to iodine deficiency, thyroid surgery, or radioiodine therapy. Risk factors for both conditions include female gender, advanced age, family history of thyroid disorders, and exposure to certain medications like lithium or amiodarone. Subclinical hypothyroidism frequently progresses to overt hypothyroidism, especially in patients with elevated thyroid-stimulating hormone (TSH) levels and positive thyroid peroxidase antibodies (TPOAb).
Common Signs and Symptoms Comparison
Subclinical hypothyroidism often presents with mild or no obvious symptoms, but may include subtle fatigue, weight gain, and cold intolerance, whereas overt hypothyroidism manifests with pronounced signs such as significant fatigue, dry skin, constipation, depression, and bradycardia. Laboratory tests in subclinical hypothyroidism show elevated TSH levels with normal free T4, while overt hypothyroidism reveals high TSH and low free T4 concentrations. Early identification of these symptom patterns along with thyroid function tests is crucial for timely diagnosis and appropriate management.
Laboratory Diagnosis and Thyroid Function Tests
Subclinical hypothyroidism is characterized by elevated thyroid-stimulating hormone (TSH) levels with normal free thyroxine (FT4) concentrations, whereas overt hypothyroidism shows elevated TSH alongside decreased FT4 levels. Thyroid function tests typically include measurements of TSH, free T4, and sometimes free triiodothyronine (FT3) to distinguish between these conditions. Accurate laboratory diagnosis is critical for guiding treatment, with high-sensitivity TSH assays essential for detecting subtle dysfunction in subclinical cases.
Health Implications of Subclinical Hypothyroidism
Subclinical hypothyroidism is characterized by elevated thyroid-stimulating hormone (TSH) levels with normal free thyroxine (T4) levels, presenting subtle or no symptoms compared to overt hypothyroidism, which involves low T4 levels and pronounced clinical features. Health implications of subclinical hypothyroidism include potential progression to overt hypothyroidism, increased risk of cardiovascular diseases, and adverse lipid profile changes. Early diagnosis and monitoring are critical to managing risks associated with subclinical hypothyroidism and preventing long-term complications.
Complications Associated with Overt Hypothyroidism
Overt hypothyroidism is associated with severe complications such as myxedema coma, cardiovascular disease including bradycardia and pericardial effusion, and significant cognitive impairment. Patients with overt hypothyroidism have a higher risk of hypercholesterolemia leading to atherosclerosis and subsequent coronary artery disease. Unlike subclinical hypothyroidism, overt hypothyroidism demands urgent medical intervention to prevent these life-threatening sequelae.
Treatment Options: Subclinical vs Overt Hypothyroidism
Subclinical hypothyroidism treatment often involves careful monitoring and may include low-dose levothyroxine therapy in patients with TSH levels above 10 mIU/L or those exhibiting symptoms, while overt hypothyroidism requires full-dose levothyroxine replacement to normalize thyroid hormone levels. Clinical guidelines recommend initiating treatment for overt hypothyroidism regardless of symptom severity due to significant risks of cardiovascular disease and myopathy. Individualized management based on TSH values, clinical presentation, and comorbidities optimizes patient outcomes in both subclinical and overt hypothyroid cases.
Long-Term Prognosis and Management Strategies
Subclinical hypothyroidism, characterized by elevated thyroid-stimulating hormone (TSH) levels with normal free thyroxine (T4), often requires regular monitoring to prevent progression to overt hypothyroidism, which presents with clear symptoms and low T4. Long-term prognosis for subclinical hypothyroidism varies, with some patients maintaining stable thyroid function while others advance to overt hypothyroidism, necessitating levothyroxine therapy to manage symptoms and prevent complications. Management strategies prioritize individualized treatment decisions based on TSH levels, age, cardiovascular risk, and presence of symptoms, with overt hypothyroidism mandating consistent thyroid hormone replacement to ensure metabolic stability and prevent morbidity.
Subclinical hypothyroidism vs overt hypothyroidism Infographic
 difterm.com
difterm.com