Autoimmune diseases occur when the immune system mistakenly attacks healthy tissues due to the presence of autoantibodies targeting specific antigens. Autoinflammatory diseases involve uncontrolled inflammation caused by innate immune system dysfunction without the presence of autoantibodies or antigen-specific T cells. Understanding the distinction between these conditions is essential for accurate diagnosis and tailored treatment strategies.
Table of Comparison
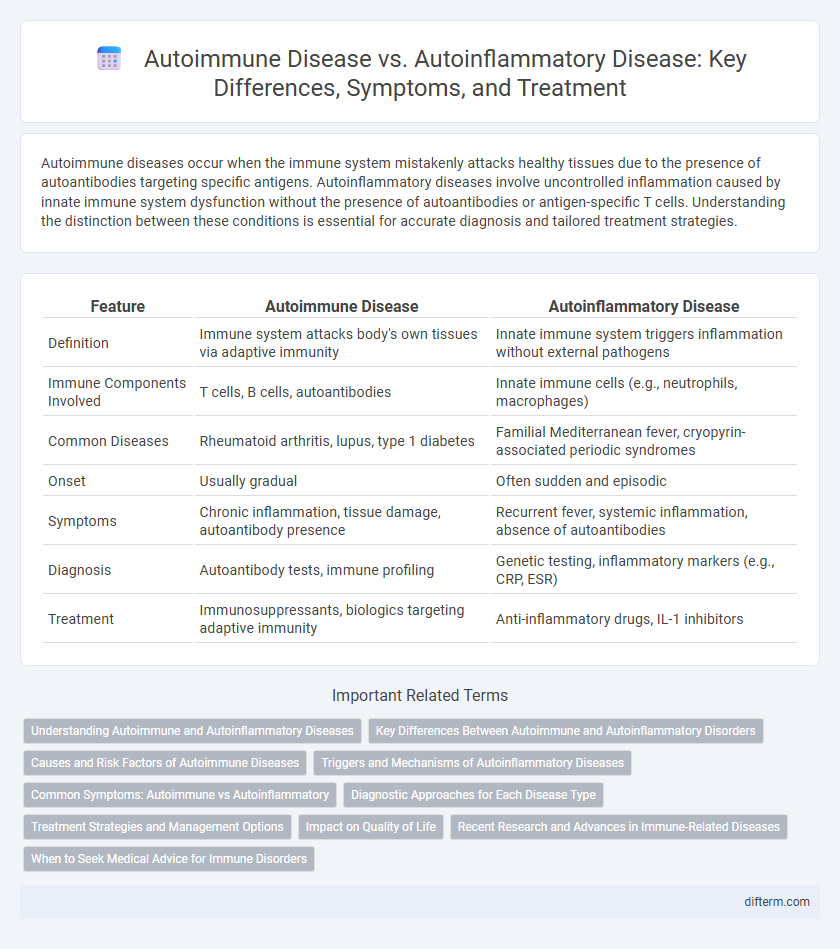
| Feature | Autoimmune Disease | Autoinflammatory Disease |
|---|---|---|
| Definition | Immune system attacks body's own tissues via adaptive immunity | Innate immune system triggers inflammation without external pathogens |
| Immune Components Involved | T cells, B cells, autoantibodies | Innate immune cells (e.g., neutrophils, macrophages) |
| Common Diseases | Rheumatoid arthritis, lupus, type 1 diabetes | Familial Mediterranean fever, cryopyrin-associated periodic syndromes |
| Onset | Usually gradual | Often sudden and episodic |
| Symptoms | Chronic inflammation, tissue damage, autoantibody presence | Recurrent fever, systemic inflammation, absence of autoantibodies |
| Diagnosis | Autoantibody tests, immune profiling | Genetic testing, inflammatory markers (e.g., CRP, ESR) |
| Treatment | Immunosuppressants, biologics targeting adaptive immunity | Anti-inflammatory drugs, IL-1 inhibitors |
Understanding Autoimmune and Autoinflammatory Diseases
Autoimmune diseases occur when the immune system mistakenly attacks the body's own tissues, involving adaptive immunity with specific autoantibodies and autoreactive T cells. Autoinflammatory diseases, in contrast, stem from innate immune system dysregulation, causing recurrent episodes of inflammation without high-titer autoantibodies or antigen-specific T cells. Understanding the distinct immunological mechanisms in autoimmune and autoinflammatory diseases is critical for accurate diagnosis and targeted therapy development.
Key Differences Between Autoimmune and Autoinflammatory Disorders
Autoimmune diseases involve adaptive immune system attacks against specific self-antigens, causing tissue damage, while autoinflammatory diseases result from innate immune system dysregulation leading to unprovoked inflammation without high-titer autoantibodies or antigen-specific T cells. Autoimmune disorders, such as rheumatoid arthritis and type 1 diabetes, typically present with autoantibodies and chronic inflammation, whereas autoinflammatory conditions like familial Mediterranean fever often feature recurrent fever episodes and systemic inflammation without these immune markers. Understanding these distinctions is crucial for accurate diagnosis and targeted treatment strategies in immune-mediated diseases.
Causes and Risk Factors of Autoimmune Diseases
Autoimmune diseases arise when the immune system mistakenly attacks healthy tissues, triggered by a combination of genetic susceptibility, environmental exposures such as infections, and hormonal influences. Family history significantly increases the risk, particularly in conditions like rheumatoid arthritis and lupus, while factors like smoking and stress can exacerbate disease onset. Understanding these causes and risk factors is crucial for early diagnosis and targeted treatment strategies in autoimmune disorders.
Triggers and Mechanisms of Autoinflammatory Diseases
Autoinflammatory diseases are primarily triggered by innate immune system dysfunction, characterized by inappropriate activation of inflammasomes leading to excessive cytokine production, such as interleukin-1b. Unlike autoimmune diseases, which involve adaptive immunity and autoantibodies targeting specific antigens, autoinflammatory diseases lack these autoantibodies and autoreactive T cells. Genetic mutations in inflammasome components, like NLRP3 or MEFV genes, drive the unchecked inflammatory response in autoinflammatory conditions.
Common Symptoms: Autoimmune vs Autoinflammatory
Common symptoms of autoimmune diseases often include fatigue, joint pain, and inflammation, as the immune system mistakenly attacks healthy tissues. Autoinflammatory diseases, in contrast, primarily cause recurrent episodes of fever, rash, and localized inflammation without the presence of autoantibodies. Both conditions involve dysregulation of the immune system but differ in underlying mechanisms and symptom presentation, requiring distinct diagnostic approaches.
Diagnostic Approaches for Each Disease Type
Autoimmune diseases are diagnosed through the detection of specific autoantibodies, tissue biopsy, and immunological assays that identify aberrant immune responses targeting the body's own tissues. Autoinflammatory diseases are primarily diagnosed using genetic testing to identify mutations in innate immune system genes, along with clinical evaluation of systemic inflammation markers such as elevated C-reactive protein (CRP) and serum amyloid A (SAA). Both disease types require differential diagnosis strategies including detailed patient history and symptom assessment to distinguish between adaptive immune-mediated autoimmunity and innate immune-driven inflammation.
Treatment Strategies and Management Options
Treatment strategies for autoimmune diseases often involve immunosuppressive drugs like corticosteroids, biologics targeting specific immune pathways, and disease-modifying antirheumatic drugs (DMARDs) to reduce immune system overactivity. Management of autoinflammatory diseases typically focuses on controlling inflammation with medications such as interleukin-1 inhibitors, nonsteroidal anti-inflammatory drugs (NSAIDs), and corticosteroids to prevent flare-ups and organ damage. Both conditions require personalized treatment plans based on disease severity, with ongoing monitoring to adjust therapies and minimize side effects.
Impact on Quality of Life
Autoimmune diseases and autoinflammatory diseases both significantly impact quality of life through chronic pain, fatigue, and fluctuating symptoms that impair daily functioning. Autoimmune conditions often involve specific organ damage and require immunosuppressive therapy, increasing the risk of infections and long-term health complications. Autoinflammatory diseases primarily cause recurrent systemic inflammation, leading to unpredictable flare-ups that disrupt physical activity, emotional well-being, and social interactions.
Recent Research and Advances in Immune-Related Diseases
Recent research in immune-related diseases has revealed distinct pathways involved in autoimmune and autoinflammatory disorders, with autoimmune diseases driven by adaptive immune system dysregulation and autoinflammatory diseases linked to innate immune system abnormalities. Advances in genomic sequencing and immunophenotyping have enabled precise identification of genetic mutations and biomarkers, facilitating personalized therapeutic approaches. Novel biologic agents targeting specific cytokines such as IL-1 and TNF-alpha demonstrate promising efficacy in modulating immune responses in both disease categories.
When to Seek Medical Advice for Immune Disorders
Persistent symptoms such as unexplained joint pain, rashes, or fatigue may indicate autoimmune diseases, necessitating prompt medical evaluation to prevent organ damage. Recurrent fevers, inflammation without infection, or unexplained swelling suggest autoinflammatory disorders requiring specialized immune system assessment. Early diagnosis through blood tests, imaging, and clinical evaluation significantly improves management outcomes for both autoimmune and autoinflammatory conditions.
autoimmune disease vs autoinflammatory disease Infographic
 difterm.com
difterm.com