Arthroscopy offers a minimally invasive approach to diagnose and treat joint issues, promoting quicker recovery and less postoperative pain compared to arthroplasty. Arthroplasty, a joint replacement procedure, is typically reserved for severe joint damage or arthritis, providing long-term pain relief and improved mobility. Choosing between arthroscopy and arthroplasty depends on the extent of joint damage, patient health, and desired outcomes.
Table of Comparison
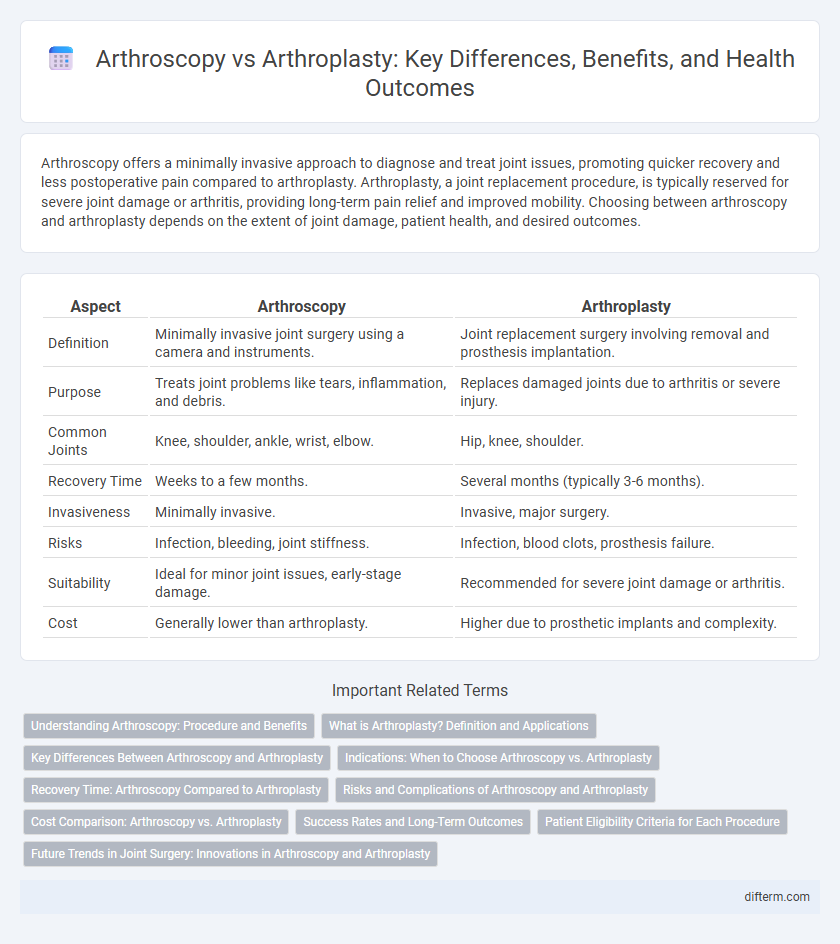
| Aspect | Arthroscopy | Arthroplasty |
|---|---|---|
| Definition | Minimally invasive joint surgery using a camera and instruments. | Joint replacement surgery involving removal and prosthesis implantation. |
| Purpose | Treats joint problems like tears, inflammation, and debris. | Replaces damaged joints due to arthritis or severe injury. |
| Common Joints | Knee, shoulder, ankle, wrist, elbow. | Hip, knee, shoulder. |
| Recovery Time | Weeks to a few months. | Several months (typically 3-6 months). |
| Invasiveness | Minimally invasive. | Invasive, major surgery. |
| Risks | Infection, bleeding, joint stiffness. | Infection, blood clots, prosthesis failure. |
| Suitability | Ideal for minor joint issues, early-stage damage. | Recommended for severe joint damage or arthritis. |
| Cost | Generally lower than arthroplasty. | Higher due to prosthetic implants and complexity. |
Understanding Arthroscopy: Procedure and Benefits
Arthroscopy is a minimally invasive surgical procedure used to diagnose and treat joint problems by inserting a small camera, called an arthroscope, into the joint through tiny incisions, allowing surgeons to view and repair damaged tissues. This technique offers benefits such as reduced pain, quicker recovery times, and less risk of infection compared to traditional open surgery. Commonly performed on knees, shoulders, and hips, arthroscopy effectively addresses issues like torn cartilage, ligament injuries, and inflammation without the extensive tissue disruption associated with arthroplasty.
What is Arthroplasty? Definition and Applications
Arthroplasty is a surgical procedure aimed at restoring joint function by resurfacing or replacing damaged joint surfaces, commonly employed to treat severe arthritis or joint trauma. It involves the partial or total replacement of a joint with prosthetic components, frequently performed on hips, knees, and shoulders to relieve pain and improve mobility. This technique is critical for patients with degenerative joint diseases where arthroscopy may be insufficient for long-term joint restoration.
Key Differences Between Arthroscopy and Arthroplasty
Arthroscopy involves minimally invasive surgery using a small camera and instruments to diagnose or treat joint issues, primarily focusing on repair and preservation of the joint. Arthroplasty, on the other hand, is a more extensive surgical procedure involving joint replacement, typically used for severe joint damage or arthritis. Key differences include recovery time, with arthroscopy offering quicker rehabilitation, while arthroplasty provides a more definitive solution for end-stage joint disease.
Indications: When to Choose Arthroscopy vs. Arthroplasty
Arthroscopy is primarily indicated for diagnosing and treating minor joint problems such as meniscal tears, ligament repairs, and early-stage cartilage damage. Arthroplasty is reserved for severe joint conditions like advanced osteoarthritis, significant joint deformities, or failed conservative treatments where joint replacement becomes necessary. Choosing between arthroscopy and arthroplasty depends on the extent of joint damage, patient age, activity level, and overall health status.
Recovery Time: Arthroscopy Compared to Arthroplasty
Arthroscopy typically allows for a faster recovery time, with patients often resuming normal activities within 4 to 6 weeks due to its minimally invasive nature. Arthroplasty, being a more extensive surgical procedure involving joint replacement, usually requires a longer rehabilitation period ranging from 3 to 6 months to regain full function. Selecting between arthroscopy and arthroplasty depends on the severity of joint damage and the desired recovery timeline.
Risks and Complications of Arthroscopy and Arthroplasty
Arthroscopy carries risks such as infection, blood clots, nerve damage, and joint stiffness, although these complications are generally less severe compared to arthroplasty. Arthroplasty, being a more invasive procedure, presents higher risks including prosthesis infection, implant loosening, deep vein thrombosis, and longer recovery times. Understanding these potential complications is crucial for patients considering surgical options for joint issues.
Cost Comparison: Arthroscopy vs. Arthroplasty
Arthroscopy generally incurs lower initial costs due to its minimally invasive nature and shorter hospital stays, with average expenses ranging from $5,000 to $10,000. Arthroplasty involves higher upfront costs, often between $20,000 and $50,000, reflecting the complexity of joint replacement surgery and extended recovery periods. Long-term cost considerations include potential revision surgeries for arthroplasty and possible ongoing treatments after arthroscopy, influencing the overall financial impact of each procedure.
Success Rates and Long-Term Outcomes
Arthroscopy typically shows high success rates for minimally invasive joint repair with quicker recovery times, particularly effective in treating meniscal tears and cartilage damage. Arthroplasty, including total joint replacement, is preferred for advanced joint degeneration, demonstrating superior long-term outcomes in pain relief and improved joint function over 10 to 20 years. Studies indicate arthroplasty has higher durability and lower revision surgery rates compared to arthroscopy for severe osteoarthritis cases.
Patient Eligibility Criteria for Each Procedure
Arthroscopy is typically recommended for patients with mild to moderate joint damage, such as meniscal tears or early-stage arthritis, who seek minimally invasive treatment with quicker recovery times. Arthroplasty suits patients with severe joint degeneration or advanced osteoarthritis, where joint replacement offers significant pain relief and improved function. Patient eligibility depends on factors like age, overall health, extent of joint damage, and activity level to determine the most appropriate surgical intervention.
Future Trends in Joint Surgery: Innovations in Arthroscopy and Arthroplasty
Emerging technologies in joint surgery emphasize minimally invasive arthroscopy combined with advancements in 3D imaging and robotic-assisted systems, enhancing precision and reducing recovery time. Arthroplasty is evolving through improved biomaterials such as bioactive ceramics and personalized implants created with 3D printing, promoting better integration and durability. These innovations are driving a shift towards tailored, patient-specific treatments that optimize functionality and long-term joint health.
arthroscopy vs arthroplasty Infographic
 difterm.com
difterm.com