Remission in health refers to the period during which symptoms of a disease decrease or disappear, indicating an improvement in the patient's condition. Relapse occurs when symptoms return or worsen after a period of remission, signaling a setback in treatment progress. Monitoring these phases closely helps in adjusting therapies and improving long-term patient outcomes.
Table of Comparison
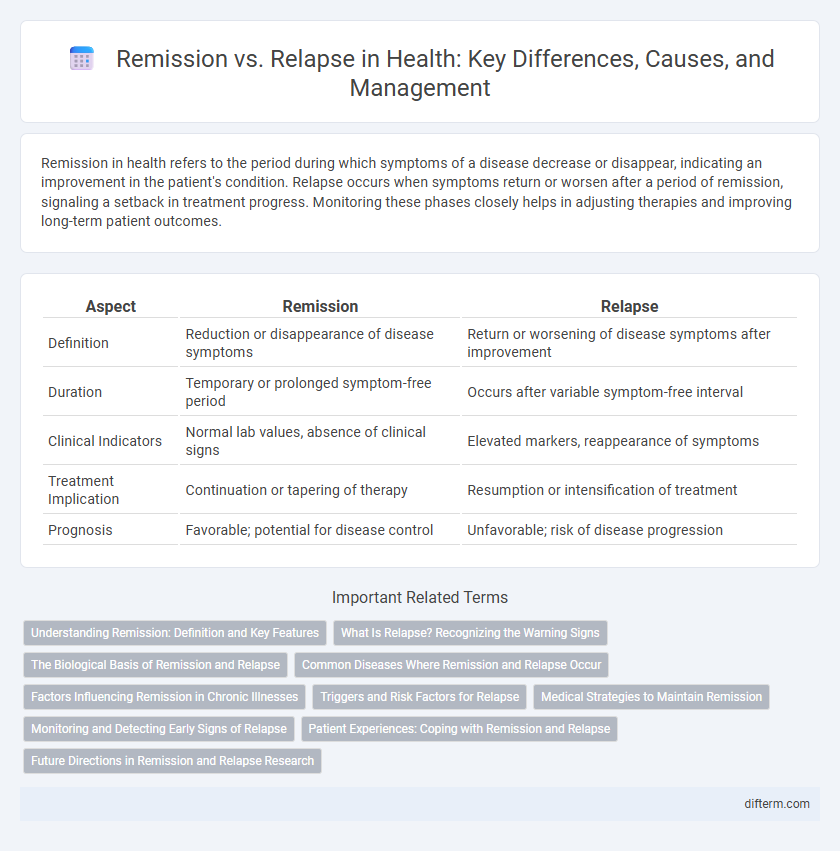
| Aspect | Remission | Relapse |
|---|---|---|
| Definition | Reduction or disappearance of disease symptoms | Return or worsening of disease symptoms after improvement |
| Duration | Temporary or prolonged symptom-free period | Occurs after variable symptom-free interval |
| Clinical Indicators | Normal lab values, absence of clinical signs | Elevated markers, reappearance of symptoms |
| Treatment Implication | Continuation or tapering of therapy | Resumption or intensification of treatment |
| Prognosis | Favorable; potential for disease control | Unfavorable; risk of disease progression |
Understanding Remission: Definition and Key Features
Remission in health refers to the period during which symptoms of a chronic illness, such as cancer or autoimmune diseases, significantly decrease or disappear, indicating an absence or reduction of active disease. Key features of remission include the absence of clinical symptoms, stabilized or improved diagnostic test results, and improved patient quality of life. Remission can be partial or complete, with complete remission indicating no detectable signs of disease and partial remission reflecting a substantial reduction in disease activity.
What Is Relapse? Recognizing the Warning Signs
Relapse occurs when symptoms of a chronic health condition, such as cancer or mental illness, return after a period of improvement or remission. Recognizing warning signs like increasing fatigue, changes in mood, or physical discomfort allows for early intervention and better management of the condition. Timely detection of relapse is crucial for adjusting treatment plans and improving patient outcomes.
The Biological Basis of Remission and Relapse
Remission occurs when disease symptoms significantly diminish due to biological factors like immune system regulation and cellular repair mechanisms restoring homeostasis. Relapse is driven by biological changes such as the reactivation of dormant pathological cells or genetic mutations that evade immune detection. Understanding these cellular and molecular processes is crucial for developing targeted therapies to sustain remission and prevent relapse.
Common Diseases Where Remission and Relapse Occur
Chronic conditions like multiple sclerosis, rheumatoid arthritis, and certain cancers frequently exhibit patterns of remission and relapse, impacting treatment strategies and patient quality of life. In autoimmune diseases such as lupus and Crohn's disease, remission phases often alternate with flare-ups, requiring continuous monitoring to manage symptoms effectively. Understanding the triggers and duration of remission and relapse in these diseases is crucial for optimizing therapeutic interventions and improving long-term outcomes.
Factors Influencing Remission in Chronic Illnesses
Factors influencing remission in chronic illnesses include effective medication adherence, lifestyle modifications such as balanced nutrition and regular exercise, and early intervention during disease flare-ups. Genetic predisposition and immune system function also play critical roles in determining the duration and stability of remission. Psychological support and stress management contribute to improved treatment outcomes and prolonged remission periods.
Triggers and Risk Factors for Relapse
Relapse in health conditions often occurs due to specific triggers such as stress, poor medication adherence, and exposure to harmful environments. Risk factors for relapse include genetic predisposition, comorbid mental health issues, and lifestyle factors like substance abuse or lack of regular medical follow-up. Identifying and managing these triggers and risk factors is critical for maintaining remission and preventing disease recurrence.
Medical Strategies to Maintain Remission
Medical strategies to maintain remission in chronic illnesses prioritize consistent medication adherence, regular monitoring through clinical assessments, and lifestyle modifications such as a balanced diet and stress management. Immunotherapy and targeted biologic treatments are increasingly used to prevent relapse by modulating the immune response. Patient education and support systems also play a crucial role in sustaining remission and improving long-term health outcomes.
Monitoring and Detecting Early Signs of Relapse
Consistent monitoring through regular medical evaluations and laboratory tests is crucial for detecting early signs of relapse in patients in remission. Biomarkers, imaging studies, and patient-reported symptoms play a vital role in identifying subtle changes that indicate disease reactivation. Early detection allows timely intervention, improving patient outcomes and prolonging remission periods.
Patient Experiences: Coping with Remission and Relapse
Patients navigating remission often experience a mix of relief and anxiety as they adjust to improved health while fearing potential relapse. Coping strategies include regular medical monitoring, mental health support, and lifestyle changes to maintain remission and manage stress. Relapse can trigger feelings of defeat, but many patients find resilience through support groups and personalized treatment plans tailored to their evolving health needs.
Future Directions in Remission and Relapse Research
Future directions in remission and relapse research emphasize the development of personalized medicine approaches using advanced genomic and biomarker analysis to predict individual patient trajectories. Innovations in real-time monitoring technologies and artificial intelligence algorithms aim to enhance early detection of relapse, enabling preemptive interventions. Collaborative efforts integrating multi-omics data and longitudinal clinical studies are critical to understanding underlying mechanisms and improving sustained remission rates in chronic diseases.
Remission vs relapse Infographic
 difterm.com
difterm.com