Primary hypertension, also known as essential hypertension, develops gradually without a specific identifiable cause and accounts for the majority of hypertension cases. Secondary hypertension results from an underlying condition such as kidney disease, hormonal disorders, or medication side effects, often presenting abruptly or with severe elevation in blood pressure. Accurate differentiation between primary and secondary hypertension is crucial for effective treatment and management strategies.
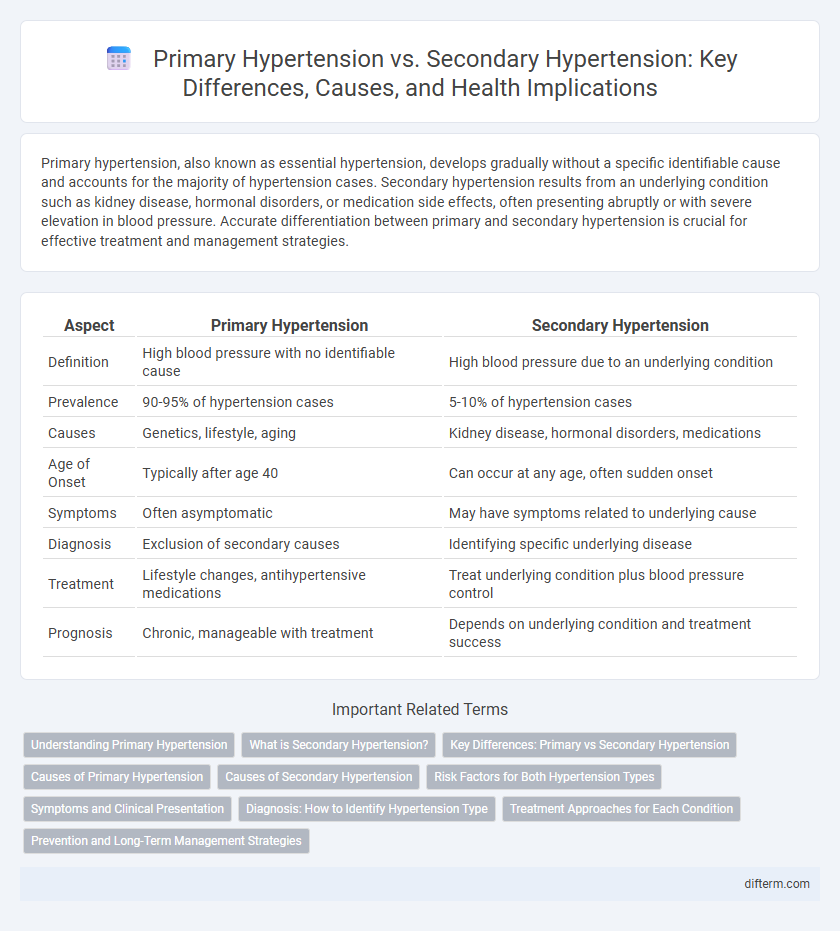
Table of Comparison
| Aspect | Primary Hypertension | Secondary Hypertension |
|---|---|---|
| Definition | High blood pressure with no identifiable cause | High blood pressure due to an underlying condition |
| Prevalence | 90-95% of hypertension cases | 5-10% of hypertension cases |
| Causes | Genetics, lifestyle, aging | Kidney disease, hormonal disorders, medications |
| Age of Onset | Typically after age 40 | Can occur at any age, often sudden onset |
| Symptoms | Often asymptomatic | May have symptoms related to underlying cause |
| Diagnosis | Exclusion of secondary causes | Identifying specific underlying disease |
| Treatment | Lifestyle changes, antihypertensive medications | Treat underlying condition plus blood pressure control |
| Prognosis | Chronic, manageable with treatment | Depends on underlying condition and treatment success |
Understanding Primary Hypertension
Primary hypertension, also known as essential hypertension, accounts for approximately 90-95% of all hypertension cases and develops gradually over years without a specific identifiable cause. It is influenced by a combination of genetic predisposition, lifestyle factors such as high sodium intake, obesity, physical inactivity, and chronic stress. Effective management relies on regular blood pressure monitoring, lifestyle modifications, and, when necessary, antihypertensive medications to reduce the risk of cardiovascular complications.
What is Secondary Hypertension?
Secondary hypertension is high blood pressure caused by an underlying medical condition such as kidney disease, hormonal disorders, or certain medications. Unlike primary hypertension, which develops gradually with no identifiable cause, secondary hypertension often appears suddenly and may be more severe. Identifying and treating the root cause of secondary hypertension is crucial to effectively manage blood pressure and reduce cardiovascular risk.
Key Differences: Primary vs Secondary Hypertension
Primary hypertension, also known as essential hypertension, accounts for approximately 90-95% of cases and arises without an identifiable medical cause, often influenced by genetic, environmental, and lifestyle factors. Secondary hypertension results from underlying conditions such as kidney disease, hormonal disorders, or medication side effects, and is less common but requires targeted treatment addressing the root cause. Accurate diagnosis differentiates primary from secondary hypertension through detailed medical history, laboratory tests, and imaging to guide effective management strategies.
Causes of Primary Hypertension
Primary hypertension, also known as essential hypertension, arises from a combination of genetic predisposition and environmental factors such as high salt intake, obesity, sedentary lifestyle, and chronic stress. Unlike secondary hypertension, which results from identifiable medical conditions like kidney disease or endocrine disorders, primary hypertension develops gradually without a specific underlying cause. This type accounts for approximately 90-95% of all hypertension cases globally, highlighting its significance in public health management.
Causes of Secondary Hypertension
Secondary hypertension is primarily caused by underlying medical conditions such as kidney disease, adrenal gland tumors, or thyroid disorders. Certain medications like corticosteroids and oral contraceptives can also trigger elevated blood pressure. Identifying these causes is crucial for targeted treatment and effective management of secondary hypertension.
Risk Factors for Both Hypertension Types
Primary hypertension is often linked to genetic predisposition, obesity, high salt intake, sedentary lifestyle, and aging. Secondary hypertension arises due to identifiable causes such as kidney disease, endocrine disorders, or medication use. Both types share common risk factors like smoking, stress, and excessive alcohol consumption, which exacerbate blood pressure elevation.
Symptoms and Clinical Presentation
Primary hypertension often presents with no specific symptoms, making it a silent condition diagnosed through consistent elevated blood pressure readings above 130/80 mm Hg. Secondary hypertension can manifest with symptoms related to underlying causes, such as headaches, sweating, palpitations, or signs of kidney disease, making clinical presentation more diverse. Recognition of symptom patterns and clinical indicators is crucial for differentiating secondary hypertension from primary forms and guiding targeted diagnostic evaluation.
Diagnosis: How to Identify Hypertension Type
Diagnosing primary versus secondary hypertension involves thorough patient history, physical examination, and targeted laboratory tests; primary hypertension is typically identified by persistently high blood pressure without an apparent cause, while secondary hypertension results from underlying conditions such as kidney disease, endocrine disorders, or medication effects. Key diagnostic procedures for secondary hypertension include renal ultrasound, aldosterone-renin ratio, and sleep studies to detect obstructive sleep apnea. Ambulatory blood pressure monitoring helps distinguish white-coat hypertension from true hypertension, guiding accurate hypertension classification.
Treatment Approaches for Each Condition
Primary hypertension treatment emphasizes lifestyle modifications such as dietary changes, regular physical activity, and weight management, often coupled with antihypertensive medications including ACE inhibitors, beta-blockers, and diuretics. Secondary hypertension management targets the underlying cause, such as adrenal gland tumors or kidney disease, with specific interventions like surgery, medication adjustment, or treatment of hormonal imbalances. Accurate diagnosis through tests like renal ultrasound or aldosterone-renin ratio is crucial to tailor effective treatment strategies.
Prevention and Long-Term Management Strategies
Primary hypertension prevention emphasizes lifestyle modifications, including a balanced diet low in sodium, regular physical activity, weight management, and stress reduction. Secondary hypertension management requires identifying and treating underlying conditions such as kidney disease, endocrine disorders, or medication side effects to effectively control blood pressure. Long-term strategies for both types involve continuous monitoring, adherence to prescribed antihypertensive medications, and regular healthcare follow-ups to prevent cardiovascular complications.
Primary hypertension vs Secondary hypertension Infographic
 difterm.com
difterm.com