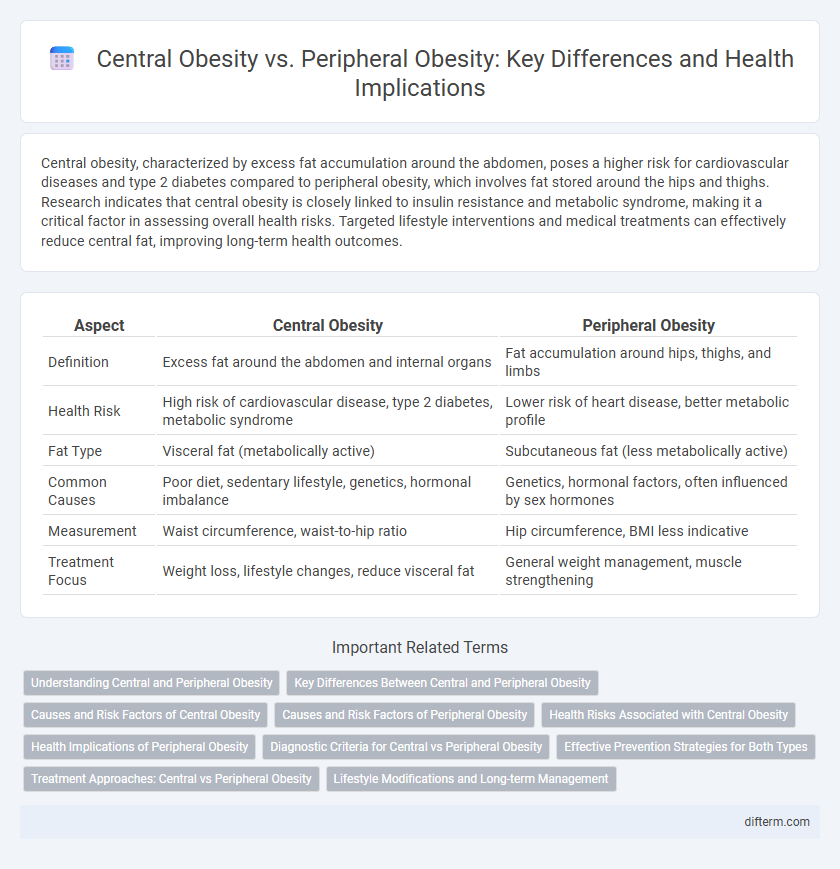
Central obesity, characterized by excess fat accumulation around the abdomen, poses a higher risk for cardiovascular diseases and type 2 diabetes compared to peripheral obesity, which involves fat stored around the hips and thighs. Research indicates that central obesity is closely linked to insulin resistance and metabolic syndrome, making it a critical factor in assessing overall health risks. Targeted lifestyle interventions and medical treatments can effectively reduce central fat, improving long-term health outcomes.
Table of Comparison
| Aspect | Central Obesity | Peripheral Obesity |
|---|---|---|
| Definition | Excess fat around the abdomen and internal organs | Fat accumulation around hips, thighs, and limbs |
| Health Risk | High risk of cardiovascular disease, type 2 diabetes, metabolic syndrome | Lower risk of heart disease, better metabolic profile |
| Fat Type | Visceral fat (metabolically active) | Subcutaneous fat (less metabolically active) |
| Common Causes | Poor diet, sedentary lifestyle, genetics, hormonal imbalance | Genetics, hormonal factors, often influenced by sex hormones |
| Measurement | Waist circumference, waist-to-hip ratio | Hip circumference, BMI less indicative |
| Treatment Focus | Weight loss, lifestyle changes, reduce visceral fat | General weight management, muscle strengthening |
Understanding Central and Peripheral Obesity
Central obesity, characterized by excessive fat accumulation around the abdomen, significantly increases the risk of cardiovascular disease, type 2 diabetes, and metabolic syndrome. Peripheral obesity involves fat deposits primarily in the hips, thighs, and buttocks, and is generally considered less harmful to metabolic health than central obesity. Understanding the distinct metabolic profiles of central and peripheral obesity aids in developing targeted interventions for managing obesity-related health risks.
Key Differences Between Central and Peripheral Obesity
Central obesity, characterized by excessive fat accumulation around the abdomen and internal organs, is strongly linked to increased risks of cardiovascular disease, type 2 diabetes, and metabolic syndrome. Peripheral obesity involves fat deposits primarily around the hips, thighs, and buttocks, posing a lower risk for metabolic complications but potentially impacting mobility and joint health. Waist-to-hip ratio and body mass index (BMI) are key metrics used to differentiate central obesity from peripheral obesity in clinical assessments.
Causes and Risk Factors of Central Obesity
Central obesity is primarily caused by excessive visceral fat accumulation around abdominal organs, driven by factors such as high-calorie diets, sedentary lifestyle, and genetic predisposition. Insulin resistance, chronic stress, and hormonal imbalances like elevated cortisol significantly contribute to increased central fat deposition. Central obesity heightens the risk of metabolic syndrome, type 2 diabetes, cardiovascular diseases, and inflammatory conditions more severely than peripheral obesity.
Causes and Risk Factors of Peripheral Obesity
Peripheral obesity is primarily caused by genetic predisposition, hormonal imbalances such as elevated estrogen levels, and lifestyle factors including sedentary behavior and high-calorie diets. Risk factors include age, particularly post-menopausal women, insulin resistance, and conditions like hypothyroidism that alter fat distribution. Unlike central obesity, peripheral fat accumulation around the hips and thighs is less associated with metabolic syndrome but can still contribute to cardiovascular risks and joint problems.
Health Risks Associated with Central Obesity
Central obesity, characterized by excess fat accumulation around the abdomen, significantly increases the risk of cardiovascular disease, type 2 diabetes, and metabolic syndrome compared to peripheral obesity, which involves fat stored in the hips and thighs. This visceral fat triggers chronic inflammation, insulin resistance, and abnormal lipid profiles, exacerbating health complications. Research shows individuals with central obesity have a two- to fourfold higher likelihood of developing heart disease and stroke than those with peripheral fat distribution.
Health Implications of Peripheral Obesity
Peripheral obesity, characterized by fat accumulation around the hips, thighs, and limbs, is associated with a lower risk of cardiovascular diseases compared to central obesity. Research indicates that subcutaneous fat in these areas promotes better lipid and glucose metabolism, reducing insulin resistance and inflammation. However, excessive peripheral fat can still contribute to musculoskeletal problems and venous insufficiency, warranting balanced body fat distribution for optimal health outcomes.
Diagnostic Criteria for Central vs Peripheral Obesity
Central obesity is primarily diagnosed through waist circumference measurements, with thresholds commonly set at >=102 cm in men and >=88 cm in women, indicating excess abdominal fat linked to higher cardiovascular risk. Peripheral obesity is assessed by evaluating fat distribution in the hips and thighs, often quantified by hip circumference or skinfold thickness, reflecting lower risk compared to central adiposity. Body mass index (BMI) alone is insufficient to distinguish between central and peripheral obesity, making regional fat assessment essential for accurate diagnosis and risk stratification.
Effective Prevention Strategies for Both Types
Effective prevention strategies for central obesity and peripheral obesity involve targeted lifestyle modifications emphasizing balanced nutrition, regular physical activity, and stress management. Incorporating a Mediterranean diet rich in fruits, vegetables, whole grains, and healthy fats supports fat distribution regulation and metabolic health. Consistent aerobic exercises combined with resistance training improve muscle mass and reduce visceral fat, while mindfulness practices lower cortisol levels, mitigating central fat accumulation risks.
Treatment Approaches: Central vs Peripheral Obesity
Treatment approaches for central obesity prioritize reducing visceral fat through lifestyle modifications like a balanced diet rich in whole grains and regular aerobic exercise, complemented by medications such as metformin or GLP-1 receptor agonists. Peripheral obesity management emphasizes increasing muscle mass and subcutaneous fat reduction through resistance training alongside targeted nutritional interventions to improve fat distribution. Both conditions benefit from personalized treatment plans addressing metabolic risk factors and promoting sustained weight loss to prevent cardiovascular diseases and type 2 diabetes.
Lifestyle Modifications and Long-term Management
Central obesity, characterized by excessive abdominal fat, significantly increases the risk of cardiovascular disease, type 2 diabetes, and metabolic syndrome, necessitating targeted lifestyle modifications such as a balanced diet low in refined sugars and regular aerobic exercise to reduce visceral fat. Peripheral obesity, involving fat accumulation around the hips and thighs, poses lower cardiometabolic risks but still benefits from strength training and dietary adjustments to improve overall metabolic health. Long-term management for both obesity types requires sustained behavioral changes, ongoing nutritional counseling, and consistent physical activity to maintain weight loss and prevent the recurrence of adiposity-related complications.
central obesity vs peripheral obesity Infographic
 difterm.com
difterm.com