Multiple myeloma and Waldenstrom macroglobulinemia are both rare types of blood cancers affecting plasma cells, but they differ in origin and symptoms. Multiple myeloma originates from malignant plasma cells in the bone marrow leading to bone damage, anemia, and kidney problems, while Waldenstrom macroglobulinemia involves abnormal B cells producing excess IgM antibody causing hyperviscosity and neuropathy. Accurate diagnosis through blood tests and bone marrow biopsy is crucial for tailoring effective treatment strategies specific to each condition.
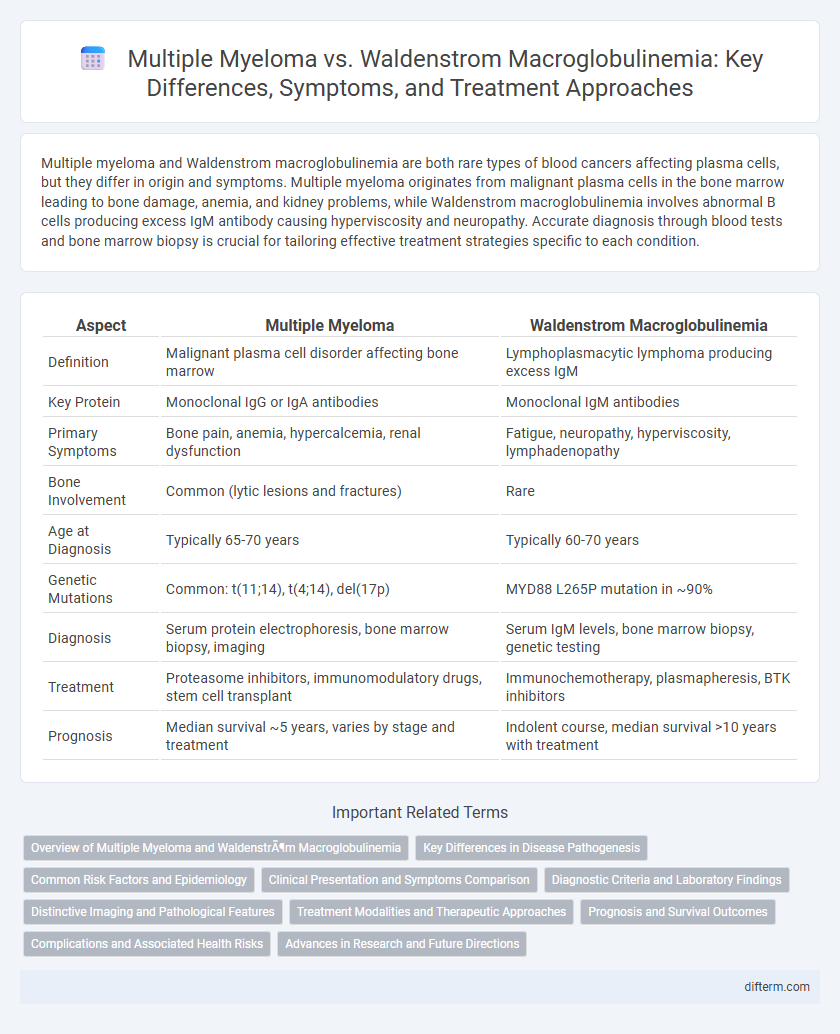
Table of Comparison
| Aspect | Multiple Myeloma | Waldenstrom Macroglobulinemia |
|---|---|---|
| Definition | Malignant plasma cell disorder affecting bone marrow | Lymphoplasmacytic lymphoma producing excess IgM |
| Key Protein | Monoclonal IgG or IgA antibodies | Monoclonal IgM antibodies |
| Primary Symptoms | Bone pain, anemia, hypercalcemia, renal dysfunction | Fatigue, neuropathy, hyperviscosity, lymphadenopathy |
| Bone Involvement | Common (lytic lesions and fractures) | Rare |
| Age at Diagnosis | Typically 65-70 years | Typically 60-70 years |
| Genetic Mutations | Common: t(11;14), t(4;14), del(17p) | MYD88 L265P mutation in ~90% |
| Diagnosis | Serum protein electrophoresis, bone marrow biopsy, imaging | Serum IgM levels, bone marrow biopsy, genetic testing |
| Treatment | Proteasome inhibitors, immunomodulatory drugs, stem cell transplant | Immunochemotherapy, plasmapheresis, BTK inhibitors |
| Prognosis | Median survival ~5 years, varies by stage and treatment | Indolent course, median survival >10 years with treatment |
Overview of Multiple Myeloma and Waldenström Macroglobulinemia
Multiple myeloma is a cancer of plasma cells characterized by the uncontrolled proliferation of malignant plasma cells in the bone marrow, leading to bone lesions, anemia, and kidney dysfunction. Waldenstrom macroglobulinemia is a rare type of non-Hodgkin lymphoma marked by the overproduction of IgM antibodies from malignant B cells, causing hyperviscosity syndrome, neuropathy, and lymphadenopathy. Both diseases involve abnormal plasma cells but differ in genetic mutations, clinical manifestations, and treatment strategies.
Key Differences in Disease Pathogenesis
Multiple myeloma is characterized by the malignant proliferation of plasma cells in the bone marrow, leading to excessive production of abnormal monoclonal immunoglobulin (M protein), primarily IgG or IgA. Waldenstrom macroglobulinemia involves the clonal expansion of lymphoplasmacytic cells producing IgM paraprotein, resulting in hyperviscosity syndrome and distinct immunopathologic features. The pathogenesis of multiple myeloma centers on genetic mutations and bone marrow microenvironment interactions, whereas Waldenstrom macroglobulinemia is driven by MYD88 L265P mutations affecting toll-like receptor signaling pathways.
Common Risk Factors and Epidemiology
Multiple myeloma primarily affects older adults, with a median diagnosis age of 69, and is more prevalent in African American populations, while Waldenstrom macroglobulinemia typically occurs in individuals over 60 and shows a higher incidence in Caucasians. Both hematologic malignancies share risk factors such as family history of lymphoproliferative disorders, exposure to certain environmental toxins, and immunosuppression. Epidemiologically, multiple myeloma accounts for about 1% of all cancers and 10% of hematologic malignancies, whereas Waldenstrom macroglobulinemia represents less than 2% of non-Hodgkin lymphomas globally.
Clinical Presentation and Symptoms Comparison
Multiple myeloma primarily presents with bone pain, anemia, hypercalcemia, and renal impairment due to malignant plasma cell proliferation in the bone marrow. Waldenstrom macroglobulinemia often manifests with symptoms related to hyperviscosity, such as blurred vision, headache, and bleeding, alongside lymphadenopathy and constitutional symptoms like fatigue and weight loss. Both disorders exhibit elevated monoclonal proteins, but the clinical presentation differs significantly based on disease pathophysiology and organ involvement.
Diagnostic Criteria and Laboratory Findings
Multiple myeloma is diagnosed through detection of clonal plasma cells exceeding 10% in bone marrow biopsy, presence of lytic bone lesions on imaging, and elevated serum monoclonal protein (M-protein) levels, predominantly IgG or IgA. Waldenstrom macroglobulinemia is characterized by lymphoplasmacytic lymphoma cells in bone marrow, IgM monoclonal gammopathy detected via serum protein electrophoresis, and hyperviscosity symptoms related to elevated IgM levels. Laboratory findings in multiple myeloma include anemia, hypercalcemia, and increased beta-2 microglobulin, whereas Waldenstrom macroglobulinemia shows elevated IgM, pancytopenia, and often increased viscosity on plasma viscosity tests.
Distinctive Imaging and Pathological Features
Multiple myeloma is characterized by lytic bone lesions visible on skeletal surveys or MRI, reflecting clonal plasma cell proliferation in the bone marrow, whereas Waldenstrom macroglobulinemia shows lymphoplasmacytic infiltration predominantly in the bone marrow without significant bone destruction. Imaging of Waldenstrom macroglobulinemia often reveals lymphadenopathy and splenomegaly on CT or PET scans, contrasting with the focal osteolytic lesions seen in multiple myeloma. Histopathologically, multiple myeloma features sheets of plasma cells with high CD138 expression, while Waldenstrom macroglobulinemia displays a mixture of small lymphocytes, plasmacytoid lymphocytes, and plasma cells with MYD88 L265P mutation present in most cases.
Treatment Modalities and Therapeutic Approaches
Multiple myeloma treatment primarily involves proteasome inhibitors, immunomodulatory drugs, and autologous stem cell transplantation, targeting malignant plasma cells in the bone marrow. Waldenstrom macroglobulinemia therapy includes rituximab-based regimens, BTK inhibitors like ibrutinib, and plasmapheresis to manage hyperviscosity caused by IgM paraproteins. Emerging treatments for both diseases focus on targeted therapies and immunotherapy to improve patient outcomes and reduce relapse rates.
Prognosis and Survival Outcomes
Multiple myeloma prognosis varies widely based on disease stage, cytogenetic abnormalities, and response to treatment, with median survival rates typically ranging from three to seven years under current therapies. Waldenstrom macroglobulinemia generally has a more indolent course, with median survival extending beyond five to ten years, although disease progression and symptomatic complications influence outcomes. Both conditions require ongoing monitoring, and advanced therapies such as targeted agents and stem cell transplantation can improve survival metrics.
Complications and Associated Health Risks
Multiple myeloma frequently leads to complications such as bone fractures, anemia, kidney dysfunction, and hypercalcemia due to malignant plasma cell proliferation. Waldenstrom macroglobulinemia primarily causes hyperviscosity syndrome, neuropathy, and increased risk of bleeding related to elevated IgM levels. Both diseases significantly impair immune function, increasing susceptibility to infections and necessitating vigilant monitoring for organ damage.
Advances in Research and Future Directions
Recent advances in research have identified distinct genetic mutations and biomarkers that differentiate multiple myeloma from Waldenstrom macroglobulinemia, enabling more precise diagnostic tools and targeted therapies. Novel immunotherapies and proteasome inhibitors show promising efficacy in multiple myeloma, while emerging BTK inhibitors and monoclonal antibodies are transforming Waldenstrom macroglobulinemia treatment landscapes. Future directions emphasize personalized medicine approaches and leveraging next-generation sequencing to improve prognosis and tailor treatment regimens for each disease.
Multiple myeloma vs Waldenström macroglobulinemia Infographic
 difterm.com
difterm.com