Metabolic syndrome in pets encompasses a cluster of conditions including obesity, hypertension, and altered lipid metabolism that increase the risk of diabetes and cardiovascular disease. Insulin resistance is a key component of metabolic syndrome, characterized by the body's reduced ability to respond to insulin, leading to elevated blood sugar levels. Early diagnosis and management of insulin resistance can prevent the progression of metabolic syndrome and improve overall pet health.
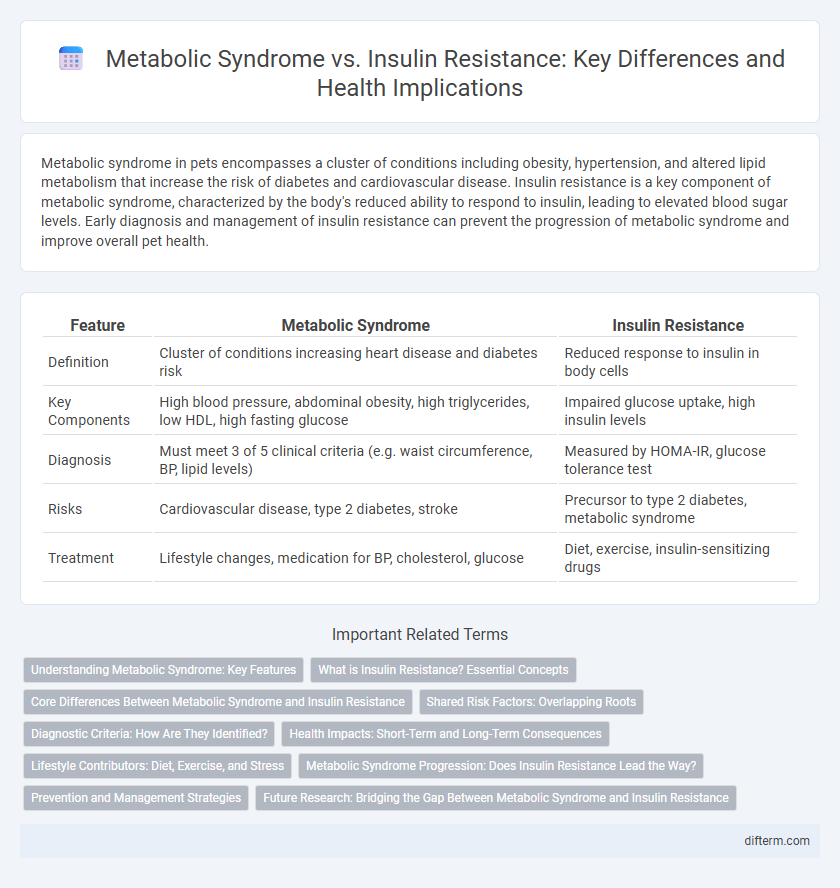
Table of Comparison
| Feature | Metabolic Syndrome | Insulin Resistance |
|---|---|---|
| Definition | Cluster of conditions increasing heart disease and diabetes risk | Reduced response to insulin in body cells |
| Key Components | High blood pressure, abdominal obesity, high triglycerides, low HDL, high fasting glucose | Impaired glucose uptake, high insulin levels |
| Diagnosis | Must meet 3 of 5 clinical criteria (e.g. waist circumference, BP, lipid levels) | Measured by HOMA-IR, glucose tolerance test |
| Risks | Cardiovascular disease, type 2 diabetes, stroke | Precursor to type 2 diabetes, metabolic syndrome |
| Treatment | Lifestyle changes, medication for BP, cholesterol, glucose | Diet, exercise, insulin-sensitizing drugs |
Understanding Metabolic Syndrome: Key Features
Metabolic syndrome is a cluster of conditions including abdominal obesity, high blood pressure, elevated fasting glucose, high triglycerides, and low HDL cholesterol, which collectively increase the risk of cardiovascular disease and type 2 diabetes. Insulin resistance, a core component of metabolic syndrome, occurs when cells fail to respond properly to insulin, leading to elevated blood sugar levels. Identifying and managing metabolic syndrome early through lifestyle changes and medical interventions can prevent severe health complications associated with insulin resistance.
What is Insulin Resistance? Essential Concepts
Insulin resistance occurs when the body's cells become less responsive to insulin, leading to elevated blood glucose levels and impaired glucose metabolism. It is a key underlying factor in the development of metabolic syndrome, which includes abdominal obesity, hypertension, dyslipidemia, and increased risk for type 2 diabetes and cardiovascular disease. Understanding insulin resistance is essential for early detection and management of metabolic health risks.
Core Differences Between Metabolic Syndrome and Insulin Resistance
Metabolic syndrome is a cluster of conditions including high blood pressure, elevated blood sugar, excess abdominal fat, and abnormal cholesterol levels, all increasing cardiovascular risk. Insulin resistance specifically refers to the body's reduced ability to respond to insulin, leading to elevated blood glucose levels. While insulin resistance can be a key underlying mechanism of metabolic syndrome, metabolic syndrome encompasses a broader range of metabolic abnormalities beyond just insulin dysfunction.
Shared Risk Factors: Overlapping Roots
Metabolic syndrome and insulin resistance share key risk factors such as obesity, physical inactivity, and a diet high in refined sugars and unhealthy fats. Both conditions involve impaired glucose metabolism and contribute to the development of type 2 diabetes and cardiovascular disease. Understanding these overlapping roots aids in early identification and intervention strategies to prevent disease progression.
Diagnostic Criteria: How Are They Identified?
Metabolic syndrome is identified through a combination of diagnostic criteria including abdominal obesity, elevated fasting glucose, hypertension, high triglycerides, and low HDL cholesterol levels. Insulin resistance is primarily diagnosed using measures such as the fasting insulin test, HOMA-IR index, or glucose tolerance tests that assess the body's response to insulin. Distinguishing between the two involves evaluating metabolic syndrome's cluster of risk factors versus insulin resistance's specific impairment in insulin signaling and glucose uptake.
Health Impacts: Short-Term and Long-Term Consequences
Metabolic syndrome significantly increases the risk of developing cardiovascular diseases, type 2 diabetes, and stroke due to persistent high blood pressure, elevated blood sugar, and abnormal cholesterol levels. Insulin resistance primarily disrupts glucose metabolism, leading to elevated blood sugar levels and potentially progressing to type 2 diabetes if untreated. Both conditions contribute to systemic inflammation and oxidative stress, exacerbating long-term complications such as organ damage and impaired cognitive function.
Lifestyle Contributors: Diet, Exercise, and Stress
Diet high in refined sugars and saturated fats significantly contributes to both metabolic syndrome and insulin resistance by promoting inflammation and adiposity. Sedentary behavior reduces muscle glucose uptake, worsening insulin sensitivity and increasing the risk of metabolic syndrome components such as hypertension and dyslipidemia. Chronic stress elevates cortisol levels, which disrupts glucose metabolism and exacerbates insulin resistance, further complicating the metabolic profile.
Metabolic Syndrome Progression: Does Insulin Resistance Lead the Way?
Metabolic syndrome progression is closely linked to insulin resistance, a condition where cells fail to respond effectively to insulin, leading to elevated blood glucose levels. Insulin resistance triggers a cascade of metabolic disturbances including increased abdominal fat, hypertension, and dyslipidemia, which collectively contribute to the development and worsening of metabolic syndrome. Monitoring insulin sensitivity is crucial for early intervention and prevention of serious complications such as type 2 diabetes and cardiovascular disease.
Prevention and Management Strategies
Effective prevention and management of metabolic syndrome and insulin resistance focus on lifestyle modifications such as adopting a balanced diet rich in whole grains, lean proteins, and healthy fats, combined with regular physical activity to improve insulin sensitivity and reduce abdominal obesity. Monitoring blood glucose levels, blood pressure, and lipid profiles aids early detection and tailored intervention, while pharmacological treatments like metformin may be prescribed to manage insulin resistance when lifestyle changes are insufficient. Emphasizing weight management, stress reduction, and smoking cessation further supports metabolic health and reduces the risk of progression to type 2 diabetes and cardiovascular disease.
Future Research: Bridging the Gap Between Metabolic Syndrome and Insulin Resistance
Future research aims to elucidate the molecular mechanisms linking metabolic syndrome and insulin resistance, enhancing early diagnostic biomarkers and personalized treatment strategies. Investigating genetic, epigenetic, and environmental factors will provide deeper insight into disease progression and potential therapeutic targets. Integrating multi-omics data and advanced machine learning models promises to bridge the current gaps in understanding these interconnected metabolic disorders.
metabolic syndrome vs insulin resistance Infographic
 difterm.com
difterm.com