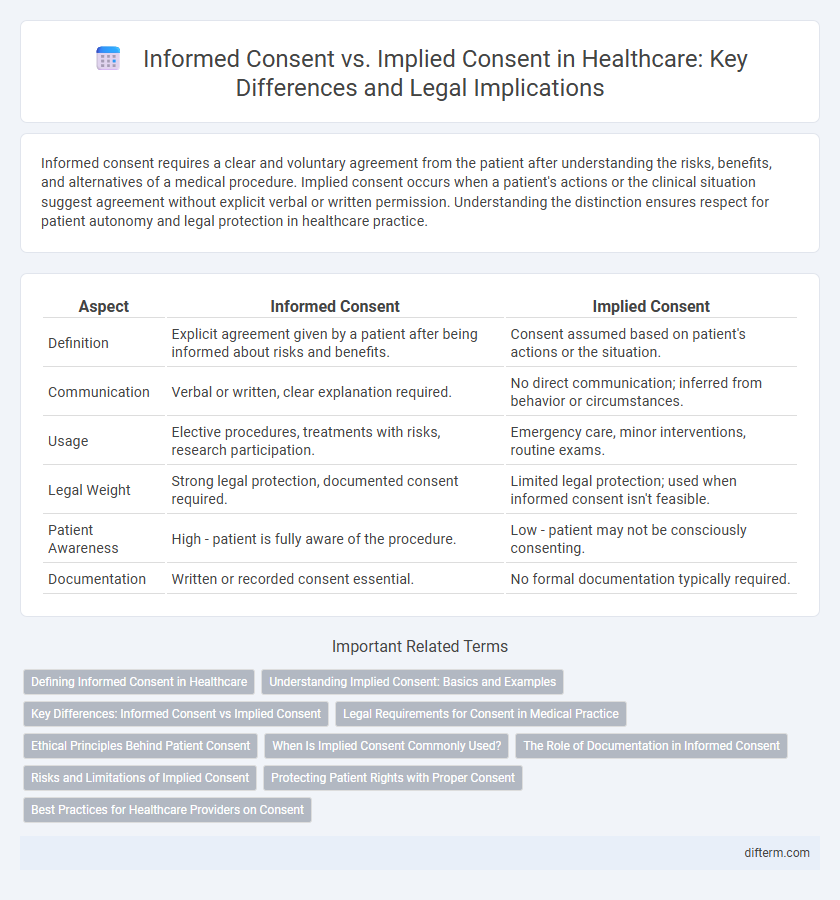
Informed consent requires a clear and voluntary agreement from the patient after understanding the risks, benefits, and alternatives of a medical procedure. Implied consent occurs when a patient's actions or the clinical situation suggest agreement without explicit verbal or written permission. Understanding the distinction ensures respect for patient autonomy and legal protection in healthcare practice.
Table of Comparison
| Aspect | Informed Consent | Implied Consent |
|---|---|---|
| Definition | Explicit agreement given by a patient after being informed about risks and benefits. | Consent assumed based on patient's actions or the situation. |
| Communication | Verbal or written, clear explanation required. | No direct communication; inferred from behavior or circumstances. |
| Usage | Elective procedures, treatments with risks, research participation. | Emergency care, minor interventions, routine exams. |
| Legal Weight | Strong legal protection, documented consent required. | Limited legal protection; used when informed consent isn't feasible. |
| Patient Awareness | High - patient is fully aware of the procedure. | Low - patient may not be consciously consenting. |
| Documentation | Written or recorded consent essential. | No formal documentation typically required. |
Defining Informed Consent in Healthcare
Informed consent in healthcare is a process where patients receive clear, comprehensive information about the benefits, risks, and alternatives of a medical procedure before agreeing to treatment. This consent ensures that the patient's decision is voluntary and based on a thorough understanding of their medical options. Unlike implied consent, which is assumed through patient behavior or circumstances, informed consent requires explicit communication and agreement.
Understanding Implied Consent: Basics and Examples
Implied consent occurs when a patient's actions or circumstances suggest agreement to medical treatment without explicit verbal or written permission, such as during emergencies where immediate care is necessary. This form of consent is common in situations where patients are unconscious or unable to communicate but require urgent interventions to prevent harm. Examples include administering CPR to an unresponsive individual or providing emergency surgery when obtaining explicit consent is impossible.
Key Differences: Informed Consent vs Implied Consent
Informed consent requires explicit permission from a patient after they receive comprehensive information about the risks, benefits, and alternatives of a medical procedure, ensuring autonomy and legal protection. Implied consent occurs when a patient's actions or circumstances suggest agreement to treatment, typically in emergencies where obtaining explicit consent is not feasible. The primary difference lies in the communication; informed consent is a documented, deliberate agreement, while implied consent is inferred from behavior or situation.
Legal Requirements for Consent in Medical Practice
Legal requirements for consent in medical practice distinguish informed consent, which mandates explicit patient agreement after comprehensive disclosure of risks, benefits, and alternatives, from implied consent, assumed through patient actions or circumstances in urgent care. Informed consent is a legal obligation supported by case law and statutory regulations ensuring patient autonomy and decision-making capacity. Implied consent applies primarily in emergency situations where immediate intervention is necessary, with documentation essential to justify the absence of explicit consent to protect healthcare providers from legal liability.
Ethical Principles Behind Patient Consent
Informed consent upholds the ethical principles of autonomy and beneficence by ensuring patients receive comprehensive information about their treatment options, risks, and benefits before agreeing to medical procedures. Implied consent relies on patients' actions or circumstances to indicate agreement, often applied in emergency situations where explicit consent is not feasible, balancing patient safety with respect for autonomy. Both consent types emphasize respect for patient dignity and promote trust in the healthcare provider-patient relationship while adhering to legal and ethical standards.
When Is Implied Consent Commonly Used?
Implied consent is commonly used in emergency medical situations where a patient is unconscious or unable to provide explicit consent, allowing healthcare providers to deliver necessary treatment without delay. It also applies when a patient voluntarily submits to a procedure, such as extending an arm for a blood draw, indicating agreement through actions rather than verbal or written consent. This form of consent ensures timely medical intervention while respecting patient autonomy in urgent or routine scenarios.
The Role of Documentation in Informed Consent
Documentation plays a crucial role in informed consent by providing a clear, legal record that the patient understands the risks, benefits, and alternatives of a medical procedure. Accurate and thorough documentation helps protect healthcare providers from liability and ensures compliance with regulatory standards such as HIPAA. In contrast, implied consent typically lacks formal documentation, making the explicit record in informed consent essential for patient rights and medical accountability.
Risks and Limitations of Implied Consent
Implied consent carries inherent risks and limitations, such as misunderstandings regarding the scope of treatment, which may lead to unauthorized procedures or patient dissatisfaction. It lacks the comprehensive documentation and explicit communication that informed consent requires, increasing legal and ethical vulnerabilities for healthcare providers. This ambiguity can compromise patient autonomy and heighten the potential for malpractice claims due to assumptions made without clear patient agreement.
Protecting Patient Rights with Proper Consent
Informed consent ensures patients are fully aware of the risks, benefits, and alternatives before undergoing medical procedures, protecting their autonomy and rights. Implied consent applies in emergencies when explicit permission cannot be obtained, assuming patient agreement based on circumstances. Proper consent protocols enhance trust and legal compliance in healthcare settings, safeguarding both patients and providers.
Best Practices for Healthcare Providers on Consent
Healthcare providers should ensure informed consent by clearly explaining procedures, risks, benefits, and alternatives to patients, securing explicit verbal or written agreement prior to treatment. Implied consent is appropriate only in emergency situations where immediate care is necessary, and obtaining explicit consent is not feasible. Best practices include documenting all consent discussions thoroughly to protect patient autonomy and comply with legal standards.
Informed consent vs implied consent Infographic
 difterm.com
difterm.com