Immunosuppression refers to the deliberate reduction of immune system activity, often induced by medications or treatments to prevent organ rejection or reduce autoimmune responses. Immunodeficiency is a condition where the immune system is inherently weakened or absent, leading to increased susceptibility to infections and diseases. Understanding the distinction between these terms is crucial for accurate diagnosis and targeted therapy in immunological disorders.
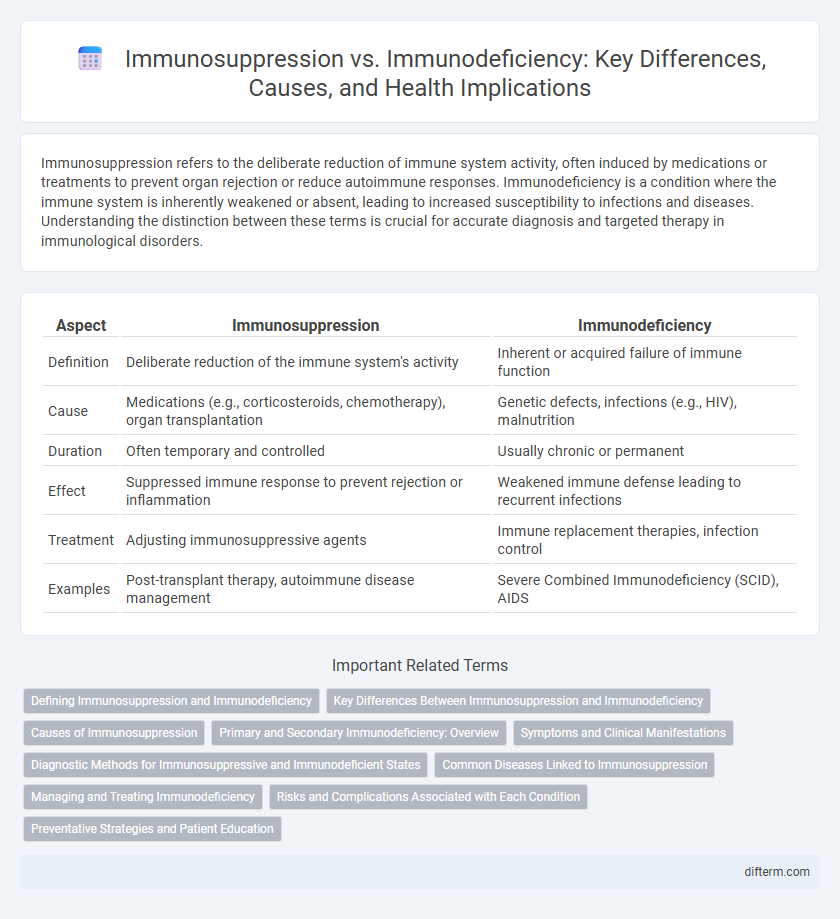
Table of Comparison
| Aspect | Immunosuppression | Immunodeficiency |
|---|---|---|
| Definition | Deliberate reduction of the immune system's activity | Inherent or acquired failure of immune function |
| Cause | Medications (e.g., corticosteroids, chemotherapy), organ transplantation | Genetic defects, infections (e.g., HIV), malnutrition |
| Duration | Often temporary and controlled | Usually chronic or permanent |
| Effect | Suppressed immune response to prevent rejection or inflammation | Weakened immune defense leading to recurrent infections |
| Treatment | Adjusting immunosuppressive agents | Immune replacement therapies, infection control |
| Examples | Post-transplant therapy, autoimmune disease management | Severe Combined Immunodeficiency (SCID), AIDS |
Defining Immunosuppression and Immunodeficiency
Immunosuppression refers to the deliberate or acquired reduction of the immune system's activity, often induced by medications like corticosteroids or caused by conditions such as organ transplantation to prevent rejection. Immunodeficiency denotes an intrinsic or acquired inability of the immune system to mount an adequate response, resulting from genetic disorders like severe combined immunodeficiency (SCID) or infections such as HIV/AIDS. Both conditions compromise immune defense but differ in etiology, with immunosuppression being a controlled suppression and immunodeficiency representing a fundamental immune system defect.
Key Differences Between Immunosuppression and Immunodeficiency
Immunosuppression refers to the deliberate reduction of immune system activity, often induced by medications like corticosteroids or chemotherapy to prevent organ transplant rejection or treat autoimmune diseases. Immunodeficiency, however, is an inherent or acquired condition characterized by the immune system's inability to mount adequate responses against infections, seen in disorders such as HIV/AIDS or primary immunodeficiency diseases. The key difference lies in immunosuppression being typically pharmacologically induced and reversible, whereas immunodeficiency involves a compromised immune function due to genetic or pathological causes.
Causes of Immunosuppression
Immunosuppression results from factors such as pharmacological agents including corticosteroids and chemotherapy drugs, infections like HIV, and diseases such as cancer that impair immune system function. Environmental exposures, malnutrition, and stress also contribute to reduced immune responsiveness. Understanding these causes is crucial for managing vulnerability to infections and improving patient outcomes.
Primary and Secondary Immunodeficiency: Overview
Primary immunodeficiency results from genetic defects impairing the immune system's ability to fight infections, often manifesting early in life with recurrent infections and autoimmune issues. Secondary immunodeficiency occurs due to external factors such as infections, malnutrition, malignancies, or immunosuppressive therapies, leading to compromised immune function in otherwise healthy individuals. Both conditions require accurate diagnosis and tailored management to prevent severe complications and improve patient outcomes.
Symptoms and Clinical Manifestations
Immunosuppression often presents with increased susceptibility to infections, delayed wound healing, and frequent reactivation of latent viruses, while immunodeficiency commonly manifests as recurrent, severe, or unusual infections due to impaired immune cell function or count. Symptoms of immunosuppression may include fatigue, fever, and opportunistic infections, whereas immunodeficiency is characterized by chronic infections, poor response to vaccines, and failure to thrive in children. Clinical manifestations in both conditions require thorough evaluation of immune parameters like lymphocyte subsets, immunoglobulin levels, and functional assays to guide diagnosis and treatment.
Diagnostic Methods for Immunosuppressive and Immunodeficient States
Diagnostic methods for immunosuppressive and immunodeficient states include a combination of immunophenotyping, flow cytometry, and measurement of immunoglobulin levels to evaluate immune cell populations and antibody production. Functional assays such as lymphocyte proliferation tests and neutrophil oxidative burst assays help assess immune response capacity, while genetic testing identifies inherited immunodeficiencies. Advanced imaging and biopsy may be employed to detect associated infections or malignancies, providing comprehensive assessment of the immune system's functionality.
Common Diseases Linked to Immunosuppression
Immunosuppression increases susceptibility to infections such as tuberculosis, cytomegalovirus, and fungal diseases like candidiasis due to weakened immune responses. Patients undergoing chemotherapy, organ transplant recipients, and individuals with HIV/AIDS commonly experience immunosuppression-related complications. These conditions heighten the risk of opportunistic infections, necessitating vigilant monitoring and preventive measures in immunosuppressed populations.
Managing and Treating Immunodeficiency
Managing and treating immunodeficiency involves personalized therapies such as immunoglobulin replacement, hematopoietic stem cell transplantation, and targeted enzyme replacement therapy to restore immune function. Regular monitoring of immune parameters and prevention of infections through vaccines and prophylactic antibiotics are critical components in optimizing patient outcomes. Advances in gene therapy and biologics offer promising avenues for durable correction of underlying genetic defects causing immunodeficiency.
Risks and Complications Associated with Each Condition
Immunosuppression involves the intentional reduction of immune system activity, commonly resulting from medications or medical treatments, increasing susceptibility to infections such as pneumonia and opportunistic pathogens like cytomegalovirus. Immunodeficiency, whether primary or acquired, leads to an inherent or chronic failure of immune defenses, heightening risks for recurrent infections, autoimmune disorders, and malignancies like lymphoma. Both conditions demand vigilant monitoring and tailored interventions to mitigate severe health complications and improve patient outcomes.
Preventative Strategies and Patient Education
Preventative strategies for immunosuppression emphasize minimizing exposure to infections through vaccination, hygiene, and safe lifestyle choices to reduce the risk of opportunistic diseases. Patient education involves informing individuals about medication adherence, recognizing early signs of infection, and maintaining routine health check-ups to enable prompt intervention. Tailored guidance on nutrition, stress management, and avoiding environmental hazards supports immune system resilience and overall health maintenance.
Immunosuppression vs immunodeficiency Infographic
 difterm.com
difterm.com