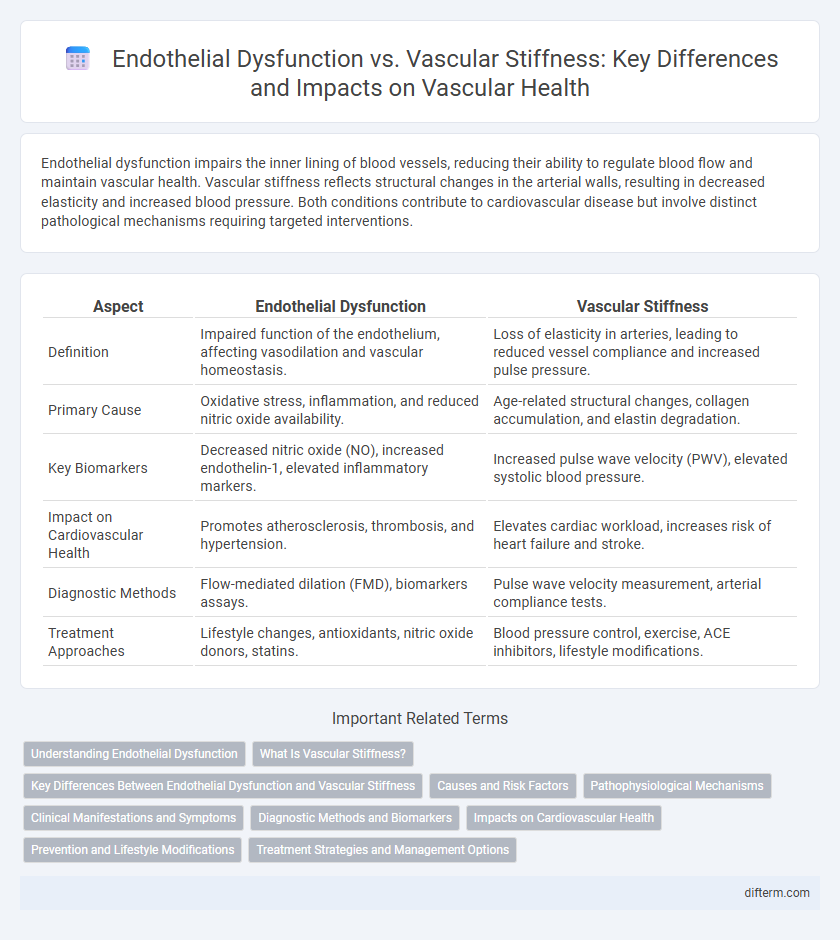
Endothelial dysfunction impairs the inner lining of blood vessels, reducing their ability to regulate blood flow and maintain vascular health. Vascular stiffness reflects structural changes in the arterial walls, resulting in decreased elasticity and increased blood pressure. Both conditions contribute to cardiovascular disease but involve distinct pathological mechanisms requiring targeted interventions.
Table of Comparison
| Aspect | Endothelial Dysfunction | Vascular Stiffness |
|---|---|---|
| Definition | Impaired function of the endothelium, affecting vasodilation and vascular homeostasis. | Loss of elasticity in arteries, leading to reduced vessel compliance and increased pulse pressure. |
| Primary Cause | Oxidative stress, inflammation, and reduced nitric oxide availability. | Age-related structural changes, collagen accumulation, and elastin degradation. |
| Key Biomarkers | Decreased nitric oxide (NO), increased endothelin-1, elevated inflammatory markers. | Increased pulse wave velocity (PWV), elevated systolic blood pressure. |
| Impact on Cardiovascular Health | Promotes atherosclerosis, thrombosis, and hypertension. | Elevates cardiac workload, increases risk of heart failure and stroke. |
| Diagnostic Methods | Flow-mediated dilation (FMD), biomarkers assays. | Pulse wave velocity measurement, arterial compliance tests. |
| Treatment Approaches | Lifestyle changes, antioxidants, nitric oxide donors, statins. | Blood pressure control, exercise, ACE inhibitors, lifestyle modifications. |
Understanding Endothelial Dysfunction
Endothelial dysfunction is a critical early marker of cardiovascular disease characterized by impaired nitric oxide production, leading to reduced vasodilation and increased inflammation. This condition disrupts the balance of vascular homeostasis, promoting arterial plaque formation and thrombosis. Understanding endothelial dysfunction helps distinguish it from vascular stiffness, which represents structural changes in the arterial wall rather than functional impairments.
What Is Vascular Stiffness?
Vascular stiffness refers to the reduced elasticity of blood vessels, primarily arteries, which impairs their ability to expand and contract with each heartbeat. This condition contributes to increased systolic blood pressure and elevated cardiac workload, significantly raising the risk of cardiovascular diseases. Measurement techniques such as pulse wave velocity (PWV) provide critical diagnostic information on arterial stiffness, aiding in early detection and management.
Key Differences Between Endothelial Dysfunction and Vascular Stiffness
Endothelial dysfunction primarily involves impaired nitric oxide production leading to reduced vasodilation, inflammation, and a pro-thrombotic state, whereas vascular stiffness refers to the loss of arterial elasticity caused by structural changes in the extracellular matrix and smooth muscle cells. Key differences include that endothelial dysfunction affects the functional regulation of blood vessels, while vascular stiffness impacts the mechanical properties and compliance of the arteries. Clinically, endothelial dysfunction is an early indicator of cardiovascular risk, while vascular stiffness contributes to increased systolic blood pressure and left ventricular workload.
Causes and Risk Factors
Endothelial dysfunction primarily results from oxidative stress, hypertension, diabetes, and smoking, impairing nitric oxide production and vascular relaxation. Vascular stiffness is mainly caused by aging, chronic inflammation, hypertension, and atherosclerosis, leading to reduced arterial compliance and increased pulse wave velocity. Both conditions share common risk factors such as obesity, sedentary lifestyle, and dyslipidemia, contributing to cardiovascular disease progression.
Pathophysiological Mechanisms
Endothelial dysfunction primarily involves impaired nitric oxide bioavailability leading to reduced vasodilation, increased oxidative stress, and inflammation, which disrupts normal vascular homeostasis. Vascular stiffness results from structural remodeling, including collagen deposition, elastin degradation, and smooth muscle cell hypertrophy, increasing arterial rigidity and pulse wave velocity. These pathophysiological mechanisms contribute synergistically to hypertension and cardiovascular disease progression by altering vessel compliance and endothelial signaling.
Clinical Manifestations and Symptoms
Endothelial dysfunction primarily manifests through impaired vasodilation, increased vascular inflammation, and elevated risk of atherosclerosis, often presenting clinically as hypertension, chest pain, and exercise intolerance. Vascular stiffness is characterized by reduced arterial elasticity, leading to increased systolic blood pressure, widened pulse pressure, and symptoms such as fatigue, dizziness, and increased cardiac workload. Both conditions contribute to cardiovascular morbidity but differ in pathophysiology and specific symptomatic presentations.
Diagnostic Methods and Biomarkers
Endothelial dysfunction is commonly assessed through flow-mediated dilation (FMD) and circulating biomarkers such as asymmetric dimethylarginine (ADMA) and endothelial microparticles, which reflect nitric oxide bioavailability and vascular inflammation. Vascular stiffness is primarily evaluated using pulse wave velocity (PWV) and augmentation index (AIx), with additional insights gained from serum markers like matrix metalloproteinases (MMPs) and elastin-derived peptides indicating extracellular matrix remodeling. Combining these diagnostic methods and biomarkers provides a comprehensive evaluation of early vascular alterations and cardiovascular risk stratification.
Impacts on Cardiovascular Health
Endothelial dysfunction impairs the production of nitric oxide, reducing vasodilation and promoting inflammation, which contributes to the progression of atherosclerosis and increased cardiovascular risk. Vascular stiffness, characterized by reduced elasticity of arterial walls, elevates systolic blood pressure and cardiac workload, resulting in left ventricular hypertrophy and higher incidence of heart failure. Both conditions synergistically exacerbate hypertension and accelerate the development of coronary artery disease and stroke.
Prevention and Lifestyle Modifications
Endothelial dysfunction and vascular stiffness both contribute significantly to cardiovascular risk, but can be effectively managed through lifestyle modifications such as regular aerobic exercise, a Mediterranean diet rich in antioxidants, and smoking cessation. Maintaining optimal blood pressure and glycemic control reduces oxidative stress and inflammation, which are key factors in preventing endothelial damage and preserving arterial elasticity. Incorporating stress management techniques like mindfulness and ensuring adequate sleep further supports vascular health by enhancing endothelial function and reducing stiffness.
Treatment Strategies and Management Options
Endothelial dysfunction treatment primarily targets restoring nitric oxide bioavailability through lifestyle changes, antioxidant therapy, and pharmacologic agents such as ACE inhibitors, statins, and PDE5 inhibitors. Vascular stiffness management focuses on controlling blood pressure with antihypertensives like calcium channel blockers and ARBs, alongside interventions to reduce arterial wall collagen cross-linking, including lifestyle modifications and emerging antifibrotic drugs. Both conditions benefit from integrated approaches involving diet, exercise, glycemic control, and smoking cessation to improve vascular health and reduce cardiovascular risk.
Endothelial Dysfunction vs Vascular Stiffness Infographic
 difterm.com
difterm.com