Aplastic anemia occurs due to bone marrow failure, resulting in insufficient production of all blood cell types, whereas hemolytic anemia is caused by the premature destruction of red blood cells. Patients with aplastic anemia often present with fatigue, infections, and bleeding due to pancytopenia, while hemolytic anemia symptoms include jaundice, dark urine, and splenomegaly. Effective diagnosis requires blood tests, bone marrow examination for aplastic anemia, and markers of red cell destruction such as increased reticulocytes and bilirubin for hemolytic anemia.
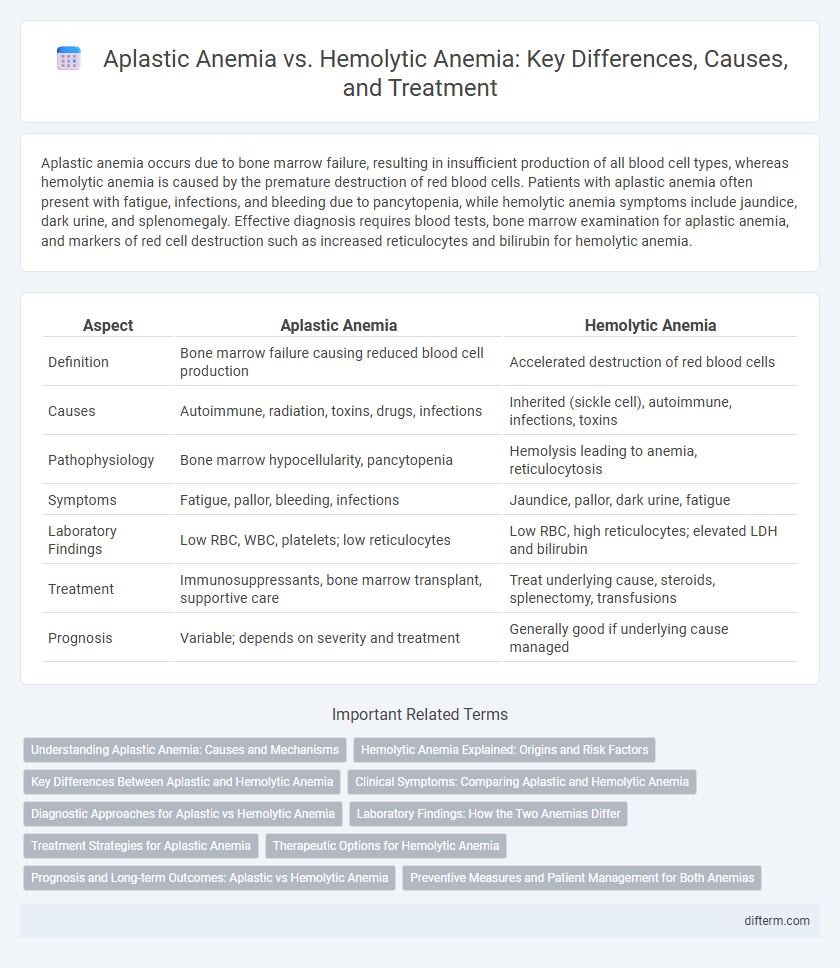
Table of Comparison
| Aspect | Aplastic Anemia | Hemolytic Anemia |
|---|---|---|
| Definition | Bone marrow failure causing reduced blood cell production | Accelerated destruction of red blood cells |
| Causes | Autoimmune, radiation, toxins, drugs, infections | Inherited (sickle cell), autoimmune, infections, toxins |
| Pathophysiology | Bone marrow hypocellularity, pancytopenia | Hemolysis leading to anemia, reticulocytosis |
| Symptoms | Fatigue, pallor, bleeding, infections | Jaundice, pallor, dark urine, fatigue |
| Laboratory Findings | Low RBC, WBC, platelets; low reticulocytes | Low RBC, high reticulocytes; elevated LDH and bilirubin |
| Treatment | Immunosuppressants, bone marrow transplant, supportive care | Treat underlying cause, steroids, splenectomy, transfusions |
| Prognosis | Variable; depends on severity and treatment | Generally good if underlying cause managed |
Understanding Aplastic Anemia: Causes and Mechanisms
Aplastic anemia is a rare bone marrow failure disorder characterized by the impaired production of all blood cell types due to damage to hematopoietic stem cells. Causes include autoimmune destruction, exposure to toxic chemicals, radiation, certain medications, and viral infections such as hepatitis and Epstein-Barr virus. Unlike hemolytic anemia, which results from premature red blood cell destruction, aplastic anemia involves a failure of the bone marrow to generate adequate blood cells, leading to pancytopenia and increased risk of infections and bleeding.
Hemolytic Anemia Explained: Origins and Risk Factors
Hemolytic anemia occurs when red blood cells are destroyed faster than the bone marrow can replace them, leading to a shortage of healthy cells. This condition can originate from inherited disorders such as sickle cell disease or acquired factors like autoimmune diseases, infections, certain medications, and exposure to toxins. Risk factors include genetic predispositions, underlying autoimmune conditions, infections such as malaria, and exposure to harmful chemicals or drugs that trigger red blood cell destruction.
Key Differences Between Aplastic and Hemolytic Anemia
Aplastic anemia is characterized by bone marrow failure leading to a deficiency in all blood cell types, while hemolytic anemia results from the premature destruction of red blood cells. Key differences include aplastic anemia's pancytopenia and hypoplastic bone marrow, contrasting with hemolytic anemia's elevated reticulocyte count and signs of increased red cell breakdown such as jaundice. Diagnostic markers like low reticulocytes and bone marrow biopsy confirm aplastic anemia, whereas hemolytic anemia shows high lactate dehydrogenase and indirect bilirubin levels.
Clinical Symptoms: Comparing Aplastic and Hemolytic Anemia
Aplastic anemia presents with clinical symptoms such as severe fatigue, frequent infections, and bleeding due to pancytopenia, reflecting bone marrow failure. Hemolytic anemia is characterized by jaundice, dark urine, and an enlarged spleen caused by the premature destruction of red blood cells. Differentiating these symptoms is critical for diagnosis and targeted treatment strategies in hematology.
Diagnostic Approaches for Aplastic vs Hemolytic Anemia
Diagnostic approaches for aplastic anemia primarily involve bone marrow biopsy revealing hypocellular marrow and pancytopenia on complete blood count, while hemolytic anemia diagnosis relies on evidence of increased red blood cell destruction, including elevated reticulocyte count, indirect hyperbilirubinemia, and positive direct Coombs test. Aplastic anemia shows low reticulocyte count and absence of hemolysis markers, contrasting with hemolytic anemia's hallmark features of hemolysis. Further laboratory tests such as lactate dehydrogenase (LDH) levels, haptoglobin, and peripheral blood smear differentiate these conditions by assessing red blood cell breakdown and marrow function.
Laboratory Findings: How the Two Anemias Differ
Aplastic anemia typically presents with pancytopenia on complete blood count, showing low red blood cells, white blood cells, and platelets, while hemolytic anemia reveals elevated reticulocyte count due to increased red blood cell destruction. Lactate dehydrogenase (LDH) and indirect bilirubin levels are significantly increased in hemolytic anemia, indicating ongoing hemolysis, whereas these markers remain normal or mildly elevated in aplastic anemia. Bone marrow biopsy in aplastic anemia shows hypocellular marrow with fatty infiltration, contrasting with a normocellular or hypercellular marrow in hemolytic anemia.
Treatment Strategies for Aplastic Anemia
Treatment strategies for aplastic anemia primarily involve immunosuppressive therapy using antithymocyte globulin (ATG) and cyclosporine, which helps restore bone marrow function by suppressing the immune attack on hematopoietic stem cells. Hematopoietic stem cell transplantation (HSCT) remains the definitive treatment, especially for younger patients with matched donors, offering the potential for long-term remission. Supportive care, including blood transfusions and infection prophylaxis, is essential to manage symptoms and complications during therapy.
Therapeutic Options for Hemolytic Anemia
Therapeutic options for hemolytic anemia primarily include corticosteroids to reduce immune system activity and immunosuppressive drugs for autoimmune cases. In severe instances, treatments such as splenectomy or intravenous immunoglobulin (IVIG) may be necessary to prevent red blood cell destruction. Supportive therapies like folic acid supplementation and blood transfusions play a crucial role in managing symptoms and improving patient outcomes.
Prognosis and Long-term Outcomes: Aplastic vs Hemolytic Anemia
Aplastic anemia generally has a more guarded prognosis due to bone marrow failure, requiring treatments such as immunosuppressive therapy or bone marrow transplantation for potential long-term remission. Hemolytic anemia often has a more favorable long-term outcome if the underlying cause is identified and managed, though chronic forms may lead to complications like splenomegaly or iron overload. Close monitoring and tailored therapeutic strategies are essential for improving survival and quality of life in both conditions.
Preventive Measures and Patient Management for Both Anemias
Preventive measures for aplastic anemia emphasize avoiding exposure to toxins like benzene and certain medications, coupled with prompt treatment of infections to minimize bone marrow damage. Hemolytic anemia prevention centers on managing autoimmune conditions and protecting against infections such as malaria that trigger red blood cell destruction. Patient management for aplastic anemia requires immunosuppressive therapy and potential bone marrow transplantation, while hemolytic anemia is managed through corticosteroids, blood transfusions, and addressing underlying causes to reduce hemolysis.
Aplastic anemia vs Hemolytic anemia Infographic
 difterm.com
difterm.com