Neutropenia specifically refers to a decreased number of neutrophils, a type of white blood cell crucial for fighting bacterial infections, while leukopenia encompasses a reduction in the total white blood cell count, including neutrophils, lymphocytes, and other immune cells. Neutropenia increases the risk of bacterial infections more directly, whereas leukopenia may indicate a broader immune deficiency affecting resistance to various pathogens. Accurate diagnosis and differentiation are essential for targeted treatment and effective management of infection risks.
Table of Comparison
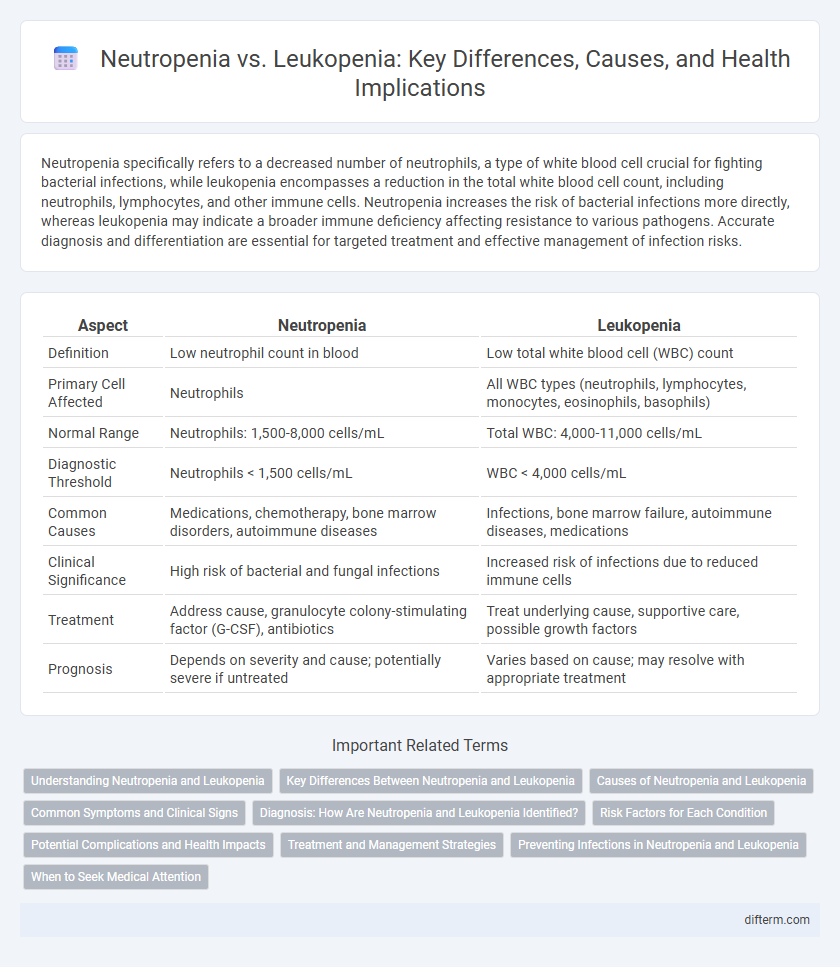
| Aspect | Neutropenia | Leukopenia |
|---|---|---|
| Definition | Low neutrophil count in blood | Low total white blood cell (WBC) count |
| Primary Cell Affected | Neutrophils | All WBC types (neutrophils, lymphocytes, monocytes, eosinophils, basophils) |
| Normal Range | Neutrophils: 1,500-8,000 cells/mL | Total WBC: 4,000-11,000 cells/mL |
| Diagnostic Threshold | Neutrophils < 1,500 cells/mL | WBC < 4,000 cells/mL |
| Common Causes | Medications, chemotherapy, bone marrow disorders, autoimmune diseases | Infections, bone marrow failure, autoimmune diseases, medications |
| Clinical Significance | High risk of bacterial and fungal infections | Increased risk of infections due to reduced immune cells |
| Treatment | Address cause, granulocyte colony-stimulating factor (G-CSF), antibiotics | Treat underlying cause, supportive care, possible growth factors |
| Prognosis | Depends on severity and cause; potentially severe if untreated | Varies based on cause; may resolve with appropriate treatment |
Understanding Neutropenia and Leukopenia
Neutropenia is characterized by an abnormally low count of neutrophils, a type of white blood cell essential for fighting bacterial infections, while leukopenia refers to a broader reduction in the total white blood cell count, including lymphocytes, monocytes, and neutrophils. Neutropenia increases vulnerability to infections, particularly bacterial and fungal, making it critical to monitor absolute neutrophil count (ANC) for diagnosis and risk assessment. Leukopenia can arise from various causes such as bone marrow disorders, autoimmune diseases, or chemotherapy, requiring detailed blood tests and bone marrow biopsy for accurate diagnosis and effective management.
Key Differences Between Neutropenia and Leukopenia
Neutropenia is characterized by an abnormally low number of neutrophils, a specific type of white blood cell essential for combating bacterial infections, while leukopenia refers to a decrease in the overall white blood cell count, including neutrophils, lymphocytes, and other white cells. The primary clinical concern in neutropenia is heightened susceptibility to bacterial and fungal infections due to neutrophil shortage, whereas leukopenia may indicate a broader immune suppression affecting multiple white cell types. Diagnosis involves complete blood count (CBC) with differential to quantify neutrophil levels for neutropenia and overall white cell count for leukopenia, guiding targeted treatment strategies based on the underlying cause.
Causes of Neutropenia and Leukopenia
Neutropenia primarily results from bone marrow disorders, chemotherapy, certain infections like HIV, and autoimmune diseases that reduce neutrophil production or increase destruction. Leukopenia encompasses a broader reduction in white blood cells caused by viral infections, severe bacterial infections, bone marrow suppression, medications, and autoimmune conditions. Identifying the underlying cause is crucial for targeted treatment and management of both neutropenia and leukopenia.
Common Symptoms and Clinical Signs
Neutropenia primarily presents with increased susceptibility to bacterial infections, often manifesting as fever, sore throat, and mouth ulcers due to low neutrophil counts. Leukopenia involves a broader reduction in white blood cells, leading to general symptoms like frequent infections, fatigue, and swollen lymph nodes. Both conditions require careful clinical evaluation to differentiate based on specific white blood cell deficits and symptom severity.
Diagnosis: How Are Neutropenia and Leukopenia Identified?
Neutropenia and leukopenia are diagnosed through a complete blood count (CBC) test, which measures the levels of white blood cells. Neutropenia is specifically identified by a low absolute neutrophil count (ANC), typically below 1,500 cells per microliter, while leukopenia refers to a decrease in total white blood cell count, often below 4,000 cells per microliter. Further diagnostic steps may include bone marrow biopsy and tests for underlying conditions to determine the cause of these abnormalities.
Risk Factors for Each Condition
Neutropenia primarily arises from chemotherapy, bone marrow disorders, or autoimmune diseases, significantly increasing the risk of bacterial and fungal infections. Leukopenia is often caused by viral infections, severe bacterial infections, or certain medications, leading to a decreased overall white blood cell count and heightened vulnerability to infections. Both conditions share overlapping risk factors such as immunosuppressive treatments and chronic illnesses but differ in the specific immune cells affected and consequent infection risks.
Potential Complications and Health Impacts
Neutropenia significantly increases the risk of bacterial and fungal infections due to reduced neutrophil levels, leading to severe complications such as sepsis and delayed wound healing. Leukopenia, characterized by a decrease in all white blood cell types, compromises the overall immune defense, heightening susceptibility to a broader range of infections and increasing morbidity in immunocompromised patients. Both conditions require prompt medical intervention to prevent life-threatening infections and ensure optimal immune function.
Treatment and Management Strategies
Treatment and management of neutropenia primarily involve addressing the underlying cause, administering granulocyte colony-stimulating factor (G-CSF) to stimulate white blood cell production, and implementing infection prevention measures such as prophylactic antibiotics. Leukopenia management focuses on identifying and treating the root cause, monitoring blood counts closely, and providing supportive care, including medications to boost immune function when necessary. Both conditions require regular hematologic evaluations and personalized treatment plans to reduce infection risk and improve patient outcomes.
Preventing Infections in Neutropenia and Leukopenia
Preventing infections in neutropenia and leukopenia requires strict hygiene practices, including frequent handwashing and avoiding contact with sick individuals due to the reduced white blood cell count impairing immune defense. Prophylactic antibiotics or antifungal agents may be prescribed to mitigate infection risk in patients with severe neutropenia, while timely vaccination can provide additional protection. Monitoring for early signs of infection and promptly seeking medical care is crucial to manage complications effectively in both conditions.
When to Seek Medical Attention
Seek medical attention immediately if neutropenia presents with a fever above 100.4degF (38degC), persistent infections, or unusual fatigue, as low neutrophil counts significantly increase infection risk. Leukopenia requiring urgent care is indicated by recurrent infections, prolonged illness, or symptoms like unexplained bruising or bleeding, signaling critical immune system compromise.
Neutropenia vs Leukopenia Infographic
 difterm.com
difterm.com