Celiac disease is an autoimmune disorder where ingesting gluten triggers an immune response that damages the small intestine, leading to nutrient malabsorption and severe health complications. Gluten sensitivity, also known as non-celiac gluten sensitivity, causes symptoms similar to celiac disease but without the autoimmune intestinal damage or positive celiac blood tests. Proper diagnosis through medical testing is essential to differentiate between these conditions and guide appropriate dietary management for improved health outcomes.
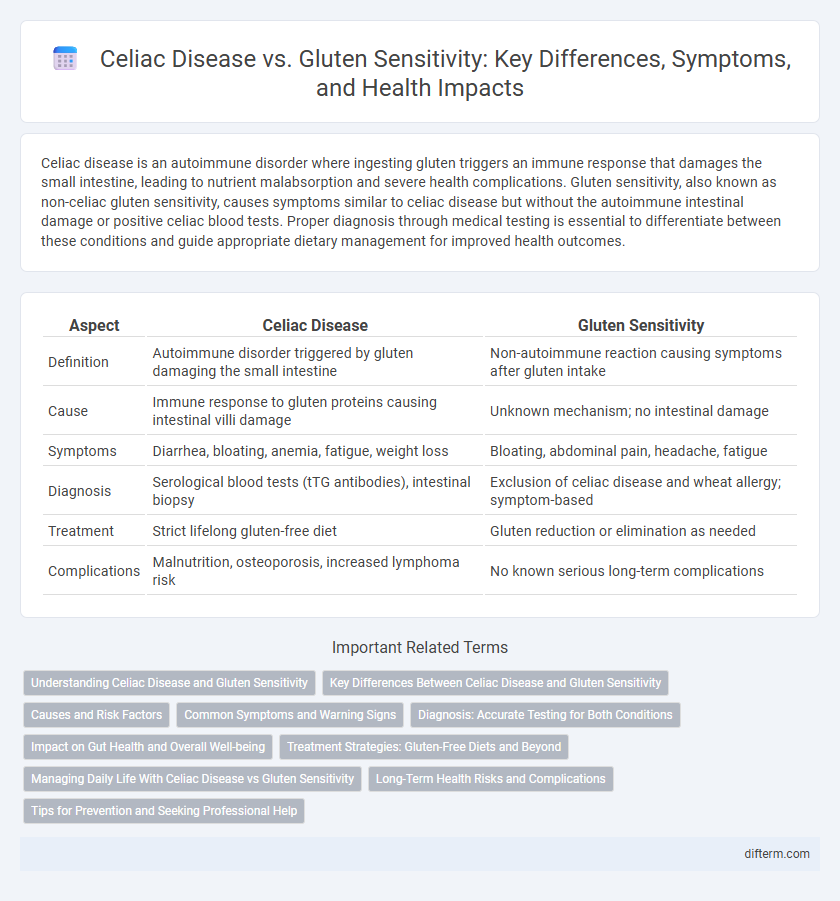
Table of Comparison
| Aspect | Celiac Disease | Gluten Sensitivity |
|---|---|---|
| Definition | Autoimmune disorder triggered by gluten damaging the small intestine | Non-autoimmune reaction causing symptoms after gluten intake |
| Cause | Immune response to gluten proteins causing intestinal villi damage | Unknown mechanism; no intestinal damage |
| Symptoms | Diarrhea, bloating, anemia, fatigue, weight loss | Bloating, abdominal pain, headache, fatigue |
| Diagnosis | Serological blood tests (tTG antibodies), intestinal biopsy | Exclusion of celiac disease and wheat allergy; symptom-based |
| Treatment | Strict lifelong gluten-free diet | Gluten reduction or elimination as needed |
| Complications | Malnutrition, osteoporosis, increased lymphoma risk | No known serious long-term complications |
Understanding Celiac Disease and Gluten Sensitivity
Celiac disease is an autoimmune disorder where ingestion of gluten triggers immune-mediated damage to the small intestine, leading to malabsorption of nutrients and symptoms like diarrhea, weight loss, and fatigue. Gluten sensitivity, also known as non-celiac gluten sensitivity, causes similar gastrointestinal and extraintestinal symptoms without the autoimmune intestinal damage or the presence of celiac-specific antibodies. Accurate diagnosis involves blood tests for celiac antibodies and intestinal biopsies for celiac disease, while gluten sensitivity is typically diagnosed by excluding celiac disease and wheat allergy after symptom improvement on a gluten-free diet.
Key Differences Between Celiac Disease and Gluten Sensitivity
Celiac disease is an autoimmune disorder triggered by gluten ingestion, causing damage to the small intestine, whereas gluten sensitivity does not involve autoimmune damage. Symptoms of celiac disease include malabsorption, nutrient deficiencies, and intestinal inflammation, while gluten sensitivity primarily presents with gastrointestinal discomfort and fatigue without intestinal injury. Diagnosis of celiac disease requires serological tests and intestinal biopsy, whereas gluten sensitivity is diagnosed mainly through symptom observation and exclusion of celiac disease.
Causes and Risk Factors
Celiac disease is triggered by an autoimmune response to gluten, primarily affecting individuals with genetic markers HLA-DQ2 or HLA-DQ8, leading to intestinal damage. Gluten sensitivity, or non-celiac gluten sensitivity (NCGS), lacks the autoimmune component and genetic markers but is caused by an adverse reaction to gluten ingestion. Risk factors for celiac disease include a family history of the condition, other autoimmune disorders, and certain environmental factors, whereas gluten sensitivity risk factors remain less clearly defined but may include gastrointestinal conditions and stress.
Common Symptoms and Warning Signs
Celiac disease and gluten sensitivity share common symptoms such as abdominal pain, bloating, diarrhea, and fatigue, but celiac disease also involves immune-mediated damage to the small intestine, detectable through blood tests for antibodies like tTG-IgA. Warning signs of celiac disease include unexplained weight loss, anemia, and nutrient deficiencies, whereas gluten sensitivity typically lacks these severe complications and intestinal damage. Early diagnosis of celiac disease is crucial to prevent long-term health issues, while gluten sensitivity management focuses on symptom relief through dietary changes.
Diagnosis: Accurate Testing for Both Conditions
Accurate diagnosis of Celiac Disease relies on serological tests such as tissue transglutaminase antibodies (tTG-IgA) and endomysial antibodies (EMA), followed by an intestinal biopsy to confirm villous atrophy. Gluten Sensitivity lacks specific biomarkers, so diagnosis is primarily based on symptom improvement after gluten elimination and exclusion of Celiac Disease and wheat allergy. Comprehensive evaluation combining clinical symptoms, serological testing, and patient history ensures precise differentiation between these gluten-related disorders.
Impact on Gut Health and Overall Well-being
Celiac disease is an autoimmune disorder where gluten ingestion leads to damage in the small intestine, significantly impairing nutrient absorption and causing symptoms such as diarrhea, bloating, and fatigue. Gluten sensitivity, although not causing intestinal damage, triggers inflammation and digestive discomfort, negatively affecting gut microbiota balance and contributing to chronic symptoms like abdominal pain and brain fog. Both conditions require dietary management to improve gut health and enhance overall well-being, but celiac disease necessitates strict lifelong gluten avoidance to prevent severe complications.
Treatment Strategies: Gluten-Free Diets and Beyond
Treatment strategies for celiac disease prioritize strict adherence to a lifelong gluten-free diet to prevent intestinal damage and associated complications. Gluten sensitivity management also involves a gluten-free diet but may allow for more flexibility and often includes monitoring symptom improvement and nutritional support. Emerging therapies beyond dietary changes, such as enzyme supplements and immune-modulating drugs, are being explored to enhance symptom control and quality of life for both conditions.
Managing Daily Life With Celiac Disease vs Gluten Sensitivity
Managing daily life with celiac disease requires strict adherence to a gluten-free diet to prevent intestinal damage and serious complications. In contrast, individuals with gluten sensitivity may tolerate small amounts of gluten without severe health risks, allowing for a more flexible dietary approach. Careful food label reading, cross-contamination prevention, and regular medical monitoring are essential for celiac patients to maintain optimal health.
Long-Term Health Risks and Complications
Celiac disease causes autoimmune damage to the small intestine, leading to malabsorption of nutrients and increasing risks of osteoporosis, anemia, and certain cancers like lymphoma over time. Gluten sensitivity, while causing discomfort and symptoms similar to celiac disease, lacks the autoimmune intestinal damage and typically does not result in severe long-term complications or increased cancer risk. Untreated celiac disease has significant long-term health consequences, making accurate diagnosis and strict gluten avoidance crucial for preventing permanent intestinal damage and related disorders.
Tips for Prevention and Seeking Professional Help
To prevent complications from celiac disease and gluten sensitivity, adhere strictly to a gluten-free diet, carefully read food labels, and avoid cross-contamination with gluten-containing products. Monitor symptoms like abdominal pain and fatigue, and consult a gastroenterologist for accurate diagnosis through serological tests and intestinal biopsy if needed. Early professional intervention helps manage symptoms effectively and reduces the risk of long-term health issues such as nutrient deficiencies and intestinal damage.
Celiac Disease vs Gluten Sensitivity Infographic
 difterm.com
difterm.com