Type 1 diabetes is an autoimmune condition where the body attacks insulin-producing cells, leading to little or no insulin production, often diagnosed in childhood or adolescence. Type 2 diabetes involves insulin resistance and is more commonly linked to lifestyle factors, typically developing in adults but increasingly seen in younger populations. Managing both types requires blood sugar monitoring, lifestyle modifications, and, in many cases, medication or insulin therapy to prevent complications.
Table of Comparison
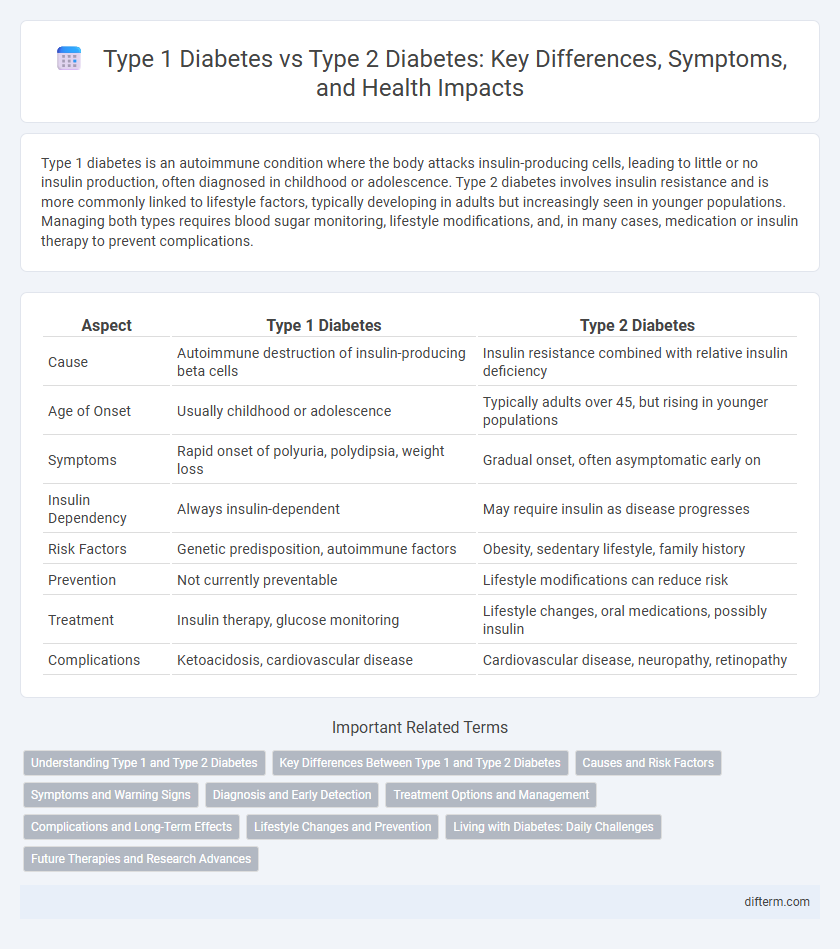
| Aspect | Type 1 Diabetes | Type 2 Diabetes |
|---|---|---|
| Cause | Autoimmune destruction of insulin-producing beta cells | Insulin resistance combined with relative insulin deficiency |
| Age of Onset | Usually childhood or adolescence | Typically adults over 45, but rising in younger populations |
| Symptoms | Rapid onset of polyuria, polydipsia, weight loss | Gradual onset, often asymptomatic early on |
| Insulin Dependency | Always insulin-dependent | May require insulin as disease progresses |
| Risk Factors | Genetic predisposition, autoimmune factors | Obesity, sedentary lifestyle, family history |
| Prevention | Not currently preventable | Lifestyle modifications can reduce risk |
| Treatment | Insulin therapy, glucose monitoring | Lifestyle changes, oral medications, possibly insulin |
| Complications | Ketoacidosis, cardiovascular disease | Cardiovascular disease, neuropathy, retinopathy |
Understanding Type 1 and Type 2 Diabetes
Type 1 diabetes is an autoimmune condition where the pancreas produces little or no insulin due to the destruction of beta cells, typically diagnosed in children and young adults. Type 2 diabetes is characterized by insulin resistance and relative insulin deficiency, often associated with obesity, aging, and lifestyle factors, and constitutes the majority of diabetes cases worldwide. Understanding the distinct pathophysiology and treatment approaches of Type 1 and Type 2 diabetes is crucial for effective disease management and preventing complications.
Key Differences Between Type 1 and Type 2 Diabetes
Type 1 diabetes is an autoimmune condition where the pancreas produces little to no insulin, typically diagnosed in children and young adults. Type 2 diabetes involves insulin resistance and relative insulin deficiency, commonly linked to obesity and lifestyle factors, often developing in adults. Key differences include the cause, age of onset, and treatment approaches, with Type 1 requiring insulin therapy and Type 2 often managed through diet, exercise, and oral medications.
Causes and Risk Factors
Type 1 Diabetes is primarily caused by an autoimmune response that destroys insulin-producing beta cells in the pancreas, with genetic predisposition playing a significant role. Type 2 Diabetes develops due to insulin resistance combined with relative insulin deficiency, strongly influenced by lifestyle factors such as obesity, physical inactivity, and poor diet. Family history, age, and ethnicity are common risk factors for both types, but modifiable behaviors largely impact Type 2 Diabetes onset.
Symptoms and Warning Signs
Type 1 diabetes symptoms include rapid weight loss, excessive thirst, frequent urination, and extreme fatigue, often appearing suddenly in children and young adults. Type 2 diabetes warning signs develop more gradually and may include blurred vision, slow-healing wounds, increased hunger, and numbness or tingling in the hands or feet. Early recognition of these symptoms is critical for timely diagnosis and effective management of both types of diabetes.
Diagnosis and Early Detection
Type 1 diabetes is diagnosed primarily through autoantibody testing and glucose level assessments, often identifying the condition in children or young adults due to its rapid onset. Type 2 diabetes diagnosis relies on fasting blood glucose tests, HbA1c levels, and oral glucose tolerance tests, with many patients detected during routine screenings or following symptoms of insulin resistance. Early detection in both types significantly improves management outcomes, highlighting the importance of regular health check-ups and monitoring high-risk individuals.
Treatment Options and Management
Type 1 Diabetes requires lifelong insulin therapy through injections or an insulin pump due to the pancreas's inability to produce insulin. In contrast, Type 2 Diabetes management often begins with lifestyle modifications such as diet and exercise, followed by oral medications like metformin, with insulin therapy introduced if blood sugar levels remain uncontrolled. Both types necessitate regular blood glucose monitoring and personalized treatment plans to prevent complications and optimize glycemic control.
Complications and Long-Term Effects
Type 1 diabetes often leads to complications such as diabetic ketoacidosis, retinopathy, nephropathy, and neuropathy due to autoimmune destruction of insulin-producing cells. Type 2 diabetes complications include cardiovascular disease, chronic kidney disease, and peripheral artery disease, primarily driven by insulin resistance and metabolic syndrome. Long-term effects in both types increase risks of stroke, limb amputations, and impaired wound healing, necessitating rigorous glucose monitoring and management.
Lifestyle Changes and Prevention
Type 1 Diabetes requires consistent insulin management and monitoring as it is an autoimmune condition, making lifestyle changes like diet and exercise supportive but not preventive. Type 2 Diabetes often develops from insulin resistance linked to obesity, physical inactivity, and poor diet, making lifestyle modifications such as maintaining a healthy weight, engaging in regular physical activity, and adopting a balanced diet critical for prevention and management. Evidence shows that individuals who adopt healthier lifestyle habits reduce their risk of developing Type 2 Diabetes by up to 58%, highlighting the importance of proactive behavioral changes.
Living with Diabetes: Daily Challenges
Living with Type 1 Diabetes requires meticulous insulin management and constant blood sugar monitoring due to the body's inability to produce insulin, demanding vigilance in diet and activity levels. Type 2 Diabetes management centers on lifestyle modifications, including weight control, balanced nutrition, and regular exercise, alongside possible oral medication or insulin therapy to enhance insulin sensitivity. Both types pose daily challenges involving symptom monitoring, preventing complications such as neuropathy or cardiovascular disease, and maintaining mental health amidst chronic disease stress.
Future Therapies and Research Advances
Emerging therapies for Type 1 Diabetes concentrate on immunotherapy and beta-cell regeneration to halt autoimmune destruction and restore insulin production. Advances in Type 2 Diabetes research emphasize personalized medicine, leveraging genetic and metabolic profiling to optimize treatment efficacy. Innovations like closed-loop insulin delivery systems and novel drug classes such as GLP-1 receptor agonists continue to transform diabetes management.
Type 1 Diabetes vs Type 2 Diabetes Infographic
 difterm.com
difterm.com