Small Intestinal Bacterial Overgrowth (SIBO) and Irritable Bowel Syndrome (IBS) share overlapping symptoms such as bloating, abdominal pain, and altered bowel habits, making differentiation challenging. SIBO involves an abnormal increase in bacteria in the small intestine, often diagnosed through breath tests measuring hydrogen or methane levels. Effective treatment depends on accurate diagnosis, with SIBO typically managed by targeted antibiotics, while IBS focuses on symptom relief through dietary changes and stress management.
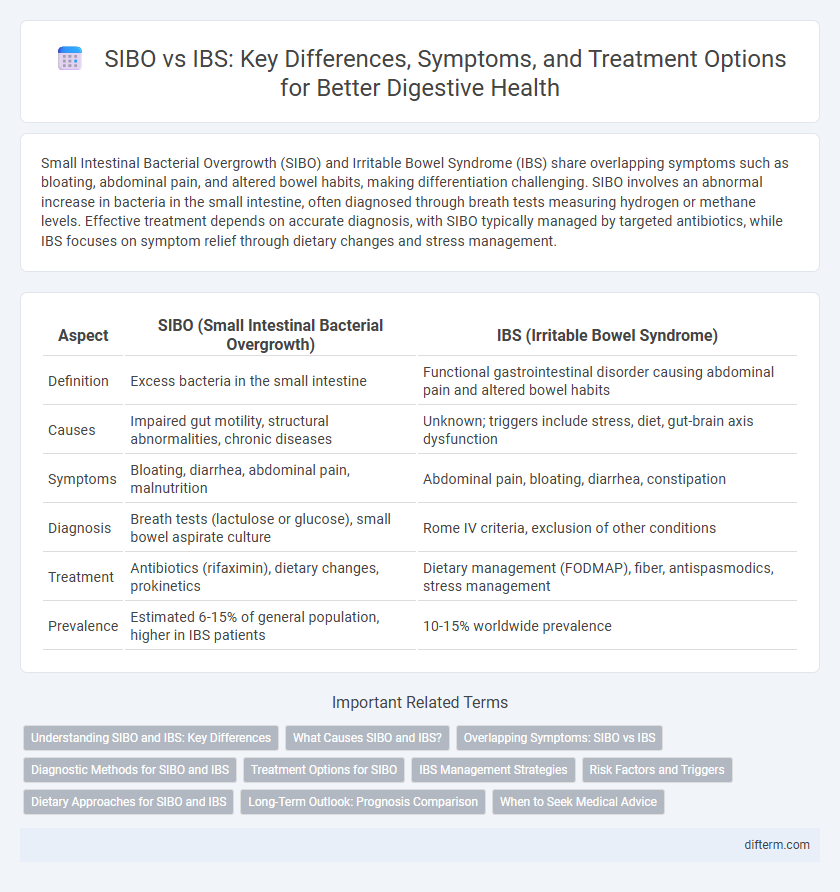
Table of Comparison
| Aspect | SIBO (Small Intestinal Bacterial Overgrowth) | IBS (Irritable Bowel Syndrome) |
|---|---|---|
| Definition | Excess bacteria in the small intestine | Functional gastrointestinal disorder causing abdominal pain and altered bowel habits |
| Causes | Impaired gut motility, structural abnormalities, chronic diseases | Unknown; triggers include stress, diet, gut-brain axis dysfunction |
| Symptoms | Bloating, diarrhea, abdominal pain, malnutrition | Abdominal pain, bloating, diarrhea, constipation |
| Diagnosis | Breath tests (lactulose or glucose), small bowel aspirate culture | Rome IV criteria, exclusion of other conditions |
| Treatment | Antibiotics (rifaximin), dietary changes, prokinetics | Dietary management (FODMAP), fiber, antispasmodics, stress management |
| Prevalence | Estimated 6-15% of general population, higher in IBS patients | 10-15% worldwide prevalence |
Understanding SIBO and IBS: Key Differences
Small Intestinal Bacterial Overgrowth (SIBO) involves an abnormal increase in bacteria in the small intestine, causing symptoms like bloating, diarrhea, and malnutrition, while Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder characterized by abdominal pain, altered bowel habits, and bloating without an identifiable cause. Diagnostic methods for SIBO include breath tests measuring hydrogen and methane gases, whereas IBS diagnosis relies on symptom-based criteria like the Rome IV guidelines. Treatment for SIBO often involves targeted antibiotics and dietary changes, contrasting with IBS management, which emphasizes symptom relief through fiber intake, stress reduction, and medications.
What Causes SIBO and IBS?
Small Intestinal Bacterial Overgrowth (SIBO) is caused by an abnormal increase of bacteria in the small intestine, often linked to factors like impaired gut motility, structural abnormalities, or use of certain medications such as proton pump inhibitors. Irritable Bowel Syndrome (IBS) arises from a complex interaction of gut-brain axis dysfunction, altered gut motility, visceral hypersensitivity, and psychosocial stressors, with contributions from dietary triggers and gut microbiota imbalances. Both conditions share overlapping symptoms but stem from distinct underlying pathophysiologies impacting gastrointestinal function.
Overlapping Symptoms: SIBO vs IBS
Small Intestinal Bacterial Overgrowth (SIBO) and Irritable Bowel Syndrome (IBS) share overlapping symptoms such as bloating, abdominal pain, diarrhea, and constipation, making differentiation challenging. Accurate diagnosis often requires breath tests for SIBO and symptom-based criteria for IBS to ensure effective treatment. Understanding the symptom overlap is crucial for targeted therapies and improving patient outcomes in gastrointestinal health.
Diagnostic Methods for SIBO and IBS
Breath tests measuring hydrogen and methane levels are the primary diagnostic tools for Small Intestinal Bacterial Overgrowth (SIBO), providing non-invasive and accurate detection of bacterial fermentation in the small intestine. In contrast, Irritable Bowel Syndrome (IBS) diagnosis relies on clinical criteria such as the Rome IV guidelines, emphasizing symptom patterns like abdominal pain and altered bowel habits, often supplemented by exclusion of other conditions through blood tests, stool analysis, and colonoscopy. Advanced diagnostics like glucose or lactulose breath tests differentiate SIBO from IBS, enabling targeted treatment strategies for these overlapping gastrointestinal disorders.
Treatment Options for SIBO
Treatment options for SIBO primarily involve targeted antibiotic therapy such as rifaximin, which helps reduce bacterial overgrowth in the small intestine. Dietary modifications, including low FODMAP and elemental diets, support symptom relief and reduce fermentable substrates for bacteria. Probiotics and herbal antimicrobials also show promise in restoring gut balance and preventing recurrence.
IBS Management Strategies
IBS management strategies emphasize dietary modifications such as low FODMAP diets to reduce symptoms like bloating and abdominal pain. Stress reduction techniques, including cognitive behavioral therapy and regular physical activity, play a crucial role in alleviating IBS symptoms. Pharmacological approaches may involve antispasmodics, laxatives, or antidiarrheals tailored to individual symptom patterns.
Risk Factors and Triggers
Small Intestinal Bacterial Overgrowth (SIBO) risk factors include impaired gut motility, previous gastrointestinal surgeries, and use of proton pump inhibitors, which disrupt normal intestinal flora. Irritable Bowel Syndrome (IBS) triggers often involve stress, dietary choices such as high FODMAP foods, and hormonal fluctuations. Understanding these distinct yet overlapping risk factors helps tailor effective treatment plans for patients experiencing chronic digestive symptoms.
Dietary Approaches for SIBO and IBS
Dietary approaches for SIBO emphasize low FODMAP and elemental diets to reduce fermentable carbohydrates that feed bacterial overgrowth, while IBS management commonly involves a low FODMAP diet to minimize gastrointestinal symptoms. SIBO-specific diets often include antimicrobial regimens combined with dietary changes to target bacterial populations, whereas IBS diets focus on symptom relief through fiber regulation and identifying trigger foods. Personalized nutrition plans based on breath tests and symptom tracking enhance outcomes for both conditions.
Long-Term Outlook: Prognosis Comparison
Small Intestinal Bacterial Overgrowth (SIBO) often shows improvement with targeted antibiotic therapy, dietary modifications, and probiotics, offering a generally favorable long-term prognosis if managed promptly. Irritable Bowel Syndrome (IBS), characterized by chronic symptom recurrence and multifactorial triggers, typically requires ongoing symptom management with lifestyle changes, medications, and psychological support, with variable long-term outcomes. Understanding the underlying causes and personalized treatment strategies significantly impacts the prognosis and quality of life for both SIBO and IBS patients.
When to Seek Medical Advice
Seek medical advice if you experience persistent bloating, abdominal pain, diarrhea, or constipation that interfere with daily activities, as these symptoms may indicate Small Intestinal Bacterial Overgrowth (SIBO) or Irritable Bowel Syndrome (IBS). Diagnostic tests such as breath tests for SIBO or colonoscopy for IBS help differentiate between the conditions and guide appropriate treatment. Early consultation with a gastroenterologist is crucial to prevent complications and improve symptom management.
SIBO vs IBS Infographic
 difterm.com
difterm.com