Non-celiac gluten sensitivity (NCGS) causes digestive and neurological symptoms triggered by gluten intake, without the intestinal damage seen in celiac disease. Celiac disease is an autoimmune disorder where gluten ingestion leads to severe small intestine inflammation and nutrient malabsorption. Accurate diagnosis through serological tests and biopsies is essential to distinguish between NCGS and celiac disease for appropriate dietary management.
Table of Comparison
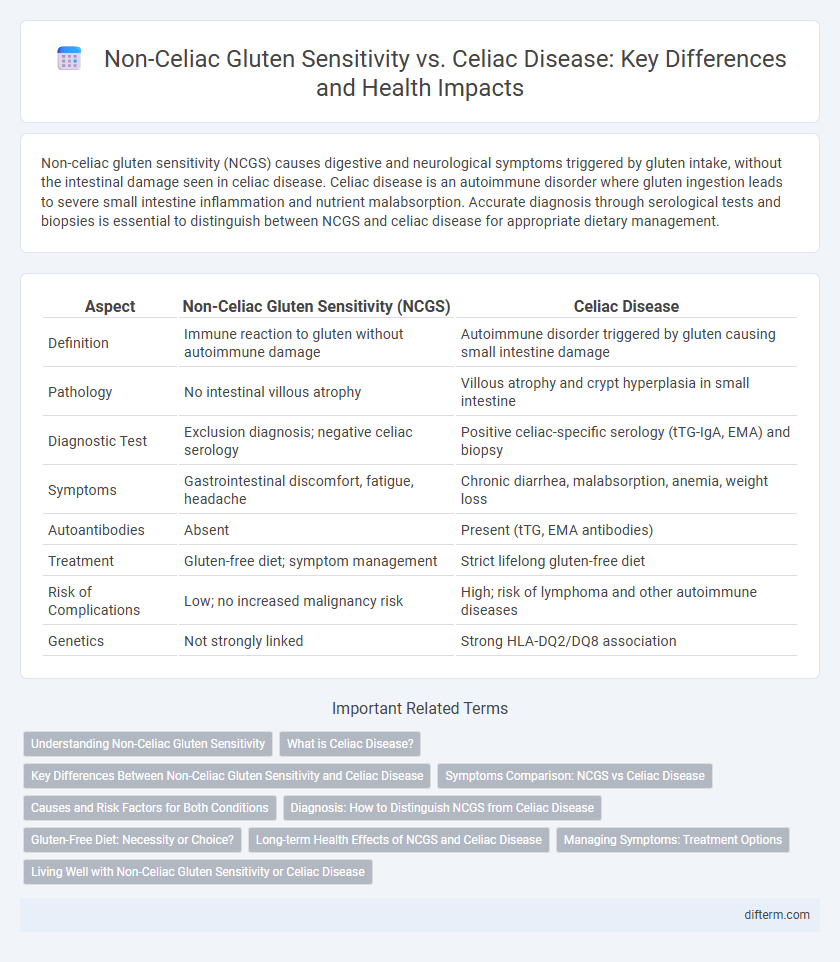
| Aspect | Non-Celiac Gluten Sensitivity (NCGS) | Celiac Disease |
|---|---|---|
| Definition | Immune reaction to gluten without autoimmune damage | Autoimmune disorder triggered by gluten causing small intestine damage |
| Pathology | No intestinal villous atrophy | Villous atrophy and crypt hyperplasia in small intestine |
| Diagnostic Test | Exclusion diagnosis; negative celiac serology | Positive celiac-specific serology (tTG-IgA, EMA) and biopsy |
| Symptoms | Gastrointestinal discomfort, fatigue, headache | Chronic diarrhea, malabsorption, anemia, weight loss |
| Autoantibodies | Absent | Present (tTG, EMA antibodies) |
| Treatment | Gluten-free diet; symptom management | Strict lifelong gluten-free diet |
| Risk of Complications | Low; no increased malignancy risk | High; risk of lymphoma and other autoimmune diseases |
| Genetics | Not strongly linked | Strong HLA-DQ2/DQ8 association |
Understanding Non-Celiac Gluten Sensitivity
Non-Celiac Gluten Sensitivity (NCGS) is characterized by adverse symptoms related to gluten ingestion without the autoimmune damage or intestinal inflammation found in Celiac disease. Unlike Celiac disease, NCGS lacks specific biomarkers such as anti-tTG antibodies or villous atrophy, making diagnosis largely clinical and symptom-based. Understanding NCGS involves recognizing its distinct immunological profile and the absence of long-term intestinal damage despite the presence of gluten-related symptoms.
What is Celiac Disease?
Celiac disease is an autoimmune disorder where ingestion of gluten triggers an immune response that damages the small intestine's lining, leading to malabsorption of nutrients. Key symptoms include diarrhea, weight loss, abdominal pain, and fatigue, and it is diagnosed through serological tests and intestinal biopsy. Strict lifelong adherence to a gluten-free diet is the only effective treatment to manage celiac disease and prevent complications such as osteoporosis and intestinal lymphoma.
Key Differences Between Non-Celiac Gluten Sensitivity and Celiac Disease
Non-celiac gluten sensitivity (NCGS) is characterized by gastrointestinal symptoms triggered by gluten ingestion without the autoimmune damage to the small intestine seen in celiac disease, which involves villous atrophy and positive anti-tTG antibodies. Unlike celiac disease, NCGS lacks specific biomarkers and does not increase the risk of long-term complications such as lymphoma or malabsorption. Diagnosis of celiac disease requires serological testing and intestinal biopsy, whereas NCGS is diagnosed mainly through symptom resolution on a gluten-free diet after celiac and wheat allergy are ruled out.
Symptoms Comparison: NCGS vs Celiac Disease
Non-celiac gluten sensitivity (NCGS) and celiac disease both manifest with gastrointestinal symptoms such as abdominal pain, bloating, and diarrhea, but celiac disease is often accompanied by more severe complications including malabsorption and nutritional deficiencies. NCGS symptoms tend to be less specific and may include extra-intestinal signs like headache, fatigue, and joint pain without the autoimmune intestinal damage seen in celiac disease. Serological markers and intestinal biopsy confirm celiac disease diagnosis, whereas NCGS is diagnosed primarily through symptom resolution on a gluten-free diet after excluding celiac disease and wheat allergy.
Causes and Risk Factors for Both Conditions
Non-celiac gluten sensitivity involves an immune response to gluten without the autoimmune damage seen in celiac disease, often triggered by gut microbiota imbalance and intestinal permeability. Celiac disease is caused by a genetic predisposition involving HLA-DQ2 or HLA-DQ8 genes, leading to an autoimmune reaction that damages the small intestine upon gluten ingestion. Both conditions share gluten exposure as a risk factor, but celiac disease has a stronger genetic link and associated autoimmune disorders.
Diagnosis: How to Distinguish NCGS from Celiac Disease
Non-celiac gluten sensitivity (NCGS) diagnosis primarily involves ruling out celiac disease and wheat allergy through serological tests such as anti-tTG and EMA antibodies, followed by an elimination diet to assess symptom improvement. In contrast, celiac disease diagnosis relies on positive serology combined with histological confirmation via duodenal biopsy showing villous atrophy and crypt hyperplasia. Genetic testing for HLA-DQ2 or HLA-DQ8 alleles supports celiac disease diagnosis but is not definitive for NCGS, which lacks specific biomarkers and requires careful clinical evaluation.
Gluten-Free Diet: Necessity or Choice?
Non-celiac gluten sensitivity (NCGS) requires a gluten-free diet primarily to alleviate symptoms like abdominal pain and fatigue, without the autoimmune damage seen in celiac disease. Celiac disease demands strict lifelong adherence to a gluten-free diet to prevent intestinal damage, nutrient malabsorption, and severe complications such as lymphoma. While both conditions benefit from gluten avoidance, the necessity of a gluten-free diet is medically imperative for celiac disease, whereas it is a personal choice for managing symptoms in NCGS.
Long-term Health Effects of NCGS and Celiac Disease
Non-celiac gluten sensitivity (NCGS) typically presents with gastrointestinal discomfort and neurological symptoms without the intestinal damage seen in celiac disease, resulting in less severe long-term health complications. Celiac disease causes chronic inflammation and villous atrophy in the small intestine, leading to malabsorption, increased risk of osteoporosis, anemia, and certain malignancies if untreated. Long-term management of both conditions involves strict gluten avoidance to prevent symptoms and potential complications, with celiac disease requiring more rigorous medical monitoring for associated autoimmune disorders.
Managing Symptoms: Treatment Options
Managing symptoms of non-celiac gluten sensitivity primarily involves adopting a gluten-free diet, which helps alleviate discomfort without the need for strict medical supervision. In contrast, celiac disease requires a lifelong adherence to a strict gluten-free diet to prevent intestinal damage and associated complications. Both conditions benefit from careful dietary planning and symptom monitoring to ensure optimal health and avoid inadvertent gluten exposure.
Living Well with Non-Celiac Gluten Sensitivity or Celiac Disease
Managing Non-Celiac Gluten Sensitivity (NCGS) involves a gluten-free diet tailored to reduce symptoms without the need for strict medical supervision required in Celiac Disease (CD). Individuals with Celiac Disease must adhere to a lifelong, strict gluten-free diet to prevent autoimmune damage to the small intestine and related complications. Both conditions benefit from regular monitoring of symptoms, nutritional support, and consultation with healthcare professionals to ensure optimal quality of life and overall health.
Non-celiac gluten sensitivity vs Celiac disease Infographic
 difterm.com
difterm.com