Atopic dermatitis is a chronic inflammatory skin condition often linked to genetic factors and immune system dysfunction, characterized by itchy, red, and dry patches frequently found on the face, inside the elbows, and behind the knees. Contact dermatitis results from direct skin exposure to irritants or allergens, causing localized redness, swelling, and blistering that typically resolves after eliminating the triggering substance. Differentiating between these conditions is crucial for effective treatment, with atopic dermatitis requiring long-term management and contact dermatitis focused on avoiding specific environmental triggers.
Table of Comparison
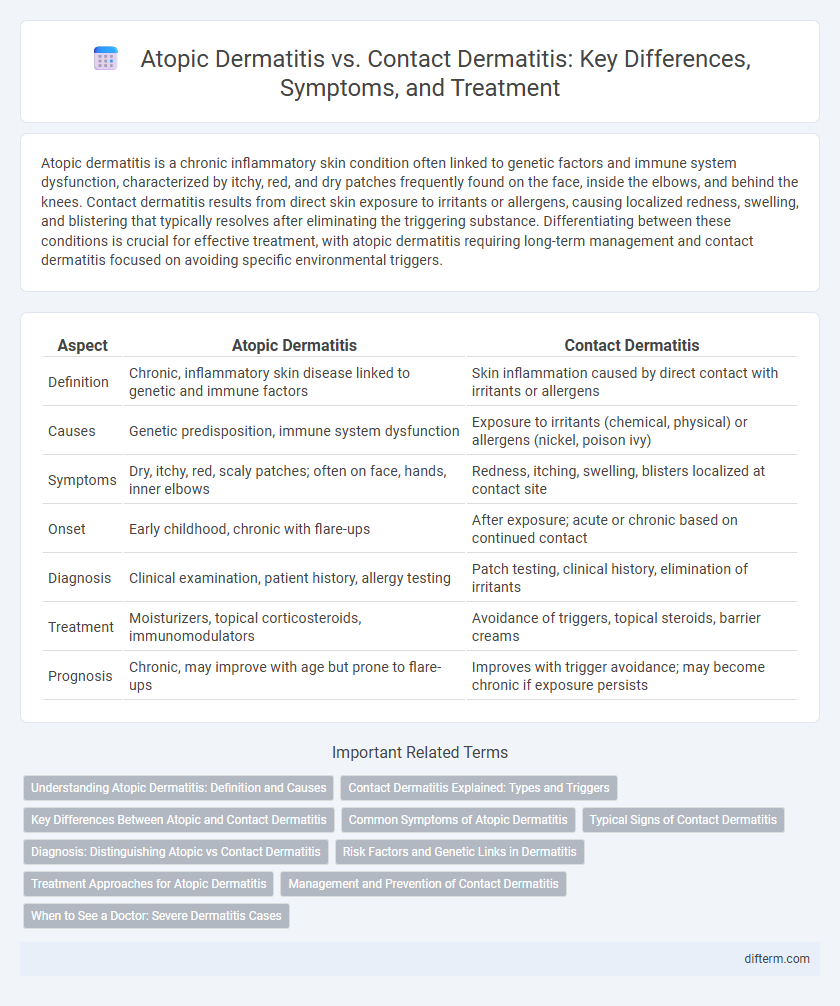
| Aspect | Atopic Dermatitis | Contact Dermatitis |
|---|---|---|
| Definition | Chronic, inflammatory skin disease linked to genetic and immune factors | Skin inflammation caused by direct contact with irritants or allergens |
| Causes | Genetic predisposition, immune system dysfunction | Exposure to irritants (chemical, physical) or allergens (nickel, poison ivy) |
| Symptoms | Dry, itchy, red, scaly patches; often on face, hands, inner elbows | Redness, itching, swelling, blisters localized at contact site |
| Onset | Early childhood, chronic with flare-ups | After exposure; acute or chronic based on continued contact |
| Diagnosis | Clinical examination, patient history, allergy testing | Patch testing, clinical history, elimination of irritants |
| Treatment | Moisturizers, topical corticosteroids, immunomodulators | Avoidance of triggers, topical steroids, barrier creams |
| Prognosis | Chronic, may improve with age but prone to flare-ups | Improves with trigger avoidance; may become chronic if exposure persists |
Understanding Atopic Dermatitis: Definition and Causes
Atopic dermatitis is a chronic inflammatory skin condition characterized by itchy, red, and dry skin, primarily caused by a combination of genetic factors and immune system dysfunction. It often begins in childhood and is associated with other atopic disorders like asthma and allergic rhinitis. Unlike contact dermatitis, which results from direct exposure to irritants or allergens, atopic dermatitis arises from an underlying predisposition to skin barrier defects and heightened immune responses.
Contact Dermatitis Explained: Types and Triggers
Contact dermatitis is an inflammatory skin condition caused by exposure to irritants or allergens, resulting in redness, itching, and blisters. The two main types are irritant contact dermatitis, triggered by substances like detergents and solvents, and allergic contact dermatitis, which occurs when the immune system reacts to allergens such as nickel, poison ivy, or fragrances. Avoiding known triggers and using barrier creams or topical corticosteroids are key strategies for managing symptoms and preventing flare-ups.
Key Differences Between Atopic and Contact Dermatitis
Atopic dermatitis is a chronic, genetic inflammatory skin condition characterized by itchy, red, and scaly patches commonly found on flexural areas, whereas contact dermatitis results from direct skin exposure to irritants or allergens causing localized inflammation and rash. Atopic dermatitis often involves systemic immune dysfunction and tends to appear early in childhood, while contact dermatitis can develop at any age following specific environmental triggers. Treatment for atopic dermatitis includes moisturizers and immune-modulating therapies, whereas contact dermatitis management focuses on identifying and avoiding the offending substances combined with topical corticosteroids.
Common Symptoms of Atopic Dermatitis
Atopic dermatitis commonly presents with intense itching, dry, scaly skin, and red, inflamed patches typically found on the face, inside the elbows, and behind the knees. This chronic condition often leads to thickened skin due to persistent scratching and may cause oozing or crusting in severe cases. Unlike contact dermatitis, which is triggered by direct skin exposure to irritants or allergens, atopic dermatitis is linked to genetic and immune system factors.
Typical Signs of Contact Dermatitis
Contact dermatitis typically presents with red, itchy rash, swelling, and blisters localized to areas directly exposed to irritants or allergens. The skin may also become dry, cracked, or scaly, often with a clear line of demarcation indicating contact with the offending substance. Unlike atopic dermatitis, contact dermatitis symptoms usually appear shortly after exposure and improve quickly once the irritant or allergen is removed.
Diagnosis: Distinguishing Atopic vs Contact Dermatitis
Diagnosis of atopic dermatitis involves identifying chronic, relapsing eczema with a history of atopy, elevated serum IgE levels, and typical flexural involvement. Contact dermatitis diagnosis requires patch testing to detect specific allergens causing localized skin reactions, often limited to areas of direct exposure. Differentiating factors include the presence of systemic allergic features in atopic dermatitis versus localized allergic or irritant responses in contact dermatitis.
Risk Factors and Genetic Links in Dermatitis
Atopic dermatitis is closely linked to genetic factors, with mutations in the filaggrin gene increasing skin barrier dysfunction and susceptibility to allergens. Contact dermatitis primarily arises from environmental exposures to irritants or allergens, with genetic predisposition playing a lesser but notable role in immune system sensitivity. Risk factors for atopic dermatitis include family history of allergies or asthma, while contact dermatitis is more common in individuals with repeated skin exposure to chemicals or metals.
Treatment Approaches for Atopic Dermatitis
Treatment approaches for atopic dermatitis primarily focus on restoring skin barrier function and reducing inflammation through regular use of emollients and topical corticosteroids. Immunomodulatory agents such as calcineurin inhibitors and newer biologics like dupilumab target underlying immune dysfunction and are effective in moderate to severe cases. Avoidance of known triggers, maintenance skincare routines, and patient education play crucial roles in preventing flare-ups and managing chronic symptoms.
Management and Prevention of Contact Dermatitis
Effective management of contact dermatitis involves identifying and avoiding specific irritants or allergens, along with the use of topical corticosteroids to reduce inflammation and itching. Preventative measures include wearing protective clothing, using barrier creams, and maintaining proper skin hydration to reinforce the skin's natural barrier. Regularly washing the skin with mild, fragrance-free cleansers helps minimize exposure to potential irritants and prevents flare-ups.
When to See a Doctor: Severe Dermatitis Cases
Seek medical attention for atopic dermatitis or contact dermatitis when symptoms include intense itching, widespread rash, swelling, or signs of infection such as pus, increased pain, or fever. Persistent flare-ups unresponsive to over-the-counter treatments and significant skin thickening or cracking also warrant professional evaluation. Early intervention by a dermatologist can prevent complications and improve long-term skin health outcomes.
Atopic dermatitis vs Contact dermatitis Infographic
 difterm.com
difterm.com