Diverticulosis involves the formation of small pouches called diverticula in the colon wall, often without symptoms. Diverticulitis occurs when these diverticula become inflamed or infected, leading to pain, fever, and digestive disturbances. Early diagnosis and treatment of diverticulitis are crucial to prevent complications like abscesses or perforation.
Table of Comparison
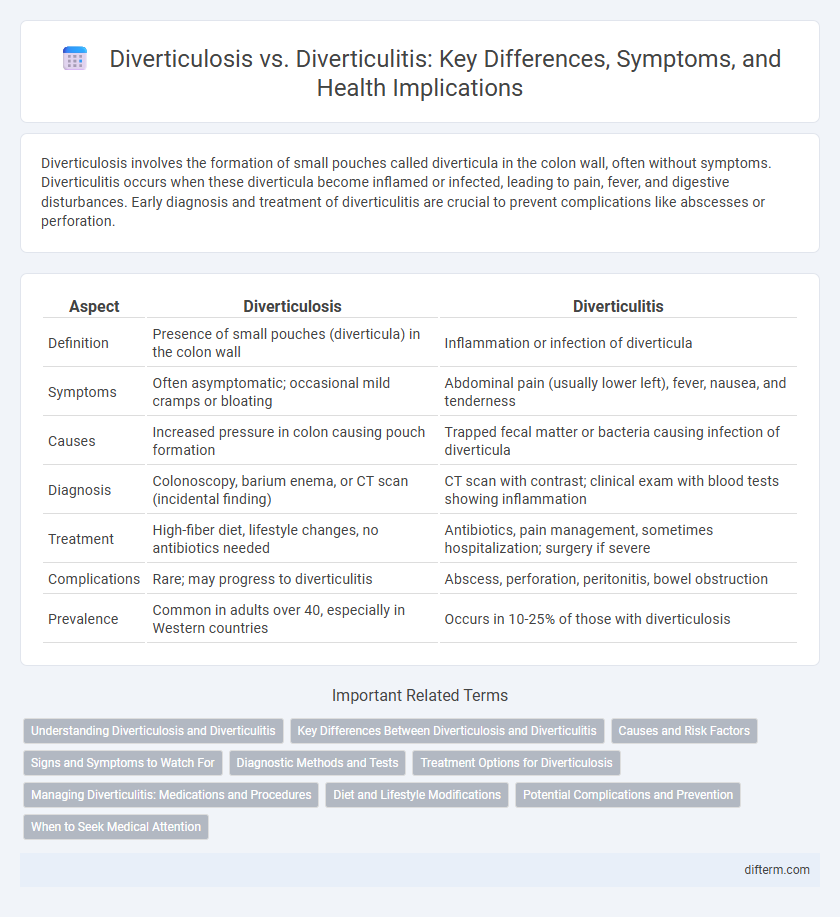
| Aspect | Diverticulosis | Diverticulitis |
|---|---|---|
| Definition | Presence of small pouches (diverticula) in the colon wall | Inflammation or infection of diverticula |
| Symptoms | Often asymptomatic; occasional mild cramps or bloating | Abdominal pain (usually lower left), fever, nausea, and tenderness |
| Causes | Increased pressure in colon causing pouch formation | Trapped fecal matter or bacteria causing infection of diverticula |
| Diagnosis | Colonoscopy, barium enema, or CT scan (incidental finding) | CT scan with contrast; clinical exam with blood tests showing inflammation |
| Treatment | High-fiber diet, lifestyle changes, no antibiotics needed | Antibiotics, pain management, sometimes hospitalization; surgery if severe |
| Complications | Rare; may progress to diverticulitis | Abscess, perforation, peritonitis, bowel obstruction |
| Prevalence | Common in adults over 40, especially in Western countries | Occurs in 10-25% of those with diverticulosis |
Understanding Diverticulosis and Diverticulitis
Diverticulosis refers to the presence of small pouches called diverticula that form in the colon wall, typically without causing symptoms. When these diverticula become inflamed or infected, the condition progresses to diverticulitis, characterized by abdominal pain, fever, and digestive disturbances. Understanding the distinction between diverticulosis and diverticulitis is critical for proper diagnosis, management, and prevention of complications such as abscesses or perforation.
Key Differences Between Diverticulosis and Diverticulitis
Diverticulosis is characterized by the formation of small pouches called diverticula in the colon wall without inflammation or symptoms, while diverticulitis occurs when these pouches become inflamed or infected, leading to abdominal pain, fever, and digestive disturbances. Diverticulosis often remains asymptomatic and is detected through colonoscopy or imaging studies, whereas diverticulitis requires prompt medical treatment to prevent complications such as abscesses or perforation. The management of diverticulosis primarily involves dietary fiber and lifestyle modifications, contrasting with the use of antibiotics and sometimes surgery in diverticulitis cases.
Causes and Risk Factors
Diverticulosis occurs when small pouches, called diverticula, form in the colon wall, primarily due to a low-fiber diet and increased pressure in the colon. Diverticulitis develops when these diverticula become inflamed or infected, often triggered by factors such as age, obesity, smoking, and lack of physical activity. Both conditions share common risk factors like advanced age and chronic constipation, but diverticulitis involves additional complications related to bacterial invasion and immune response.
Signs and Symptoms to Watch For
Diverticulosis often presents with mild or no symptoms, but may include occasional abdominal cramping or bloating, primarily in the lower left abdomen. Diverticulitis symptoms are more acute, featuring severe abdominal pain, fever, nausea, constipation, or diarrhea. Recognizing these signs early is crucial to prevent complications such as infection or bowel obstruction.
Diagnostic Methods and Tests
Diverticulosis is typically diagnosed through colonoscopy or CT colonography, revealing small pouches in the colon wall without inflammation. Diverticulitis diagnosis relies heavily on abdominal CT scans with contrast, which identify inflamed or infected diverticula and complications such as abscesses. Blood tests may show elevated white blood cell counts in diverticulitis, aiding differentiation from asymptomatic diverticulosis.
Treatment Options for Diverticulosis
Treatment options for diverticulosis primarily focus on dietary modifications, including a high-fiber diet to promote regular bowel movements and prevent the formation of new diverticula. Increasing water intake and incorporating fiber supplements like psyllium can further reduce symptoms and complications. In some cases, healthcare providers may recommend probiotics to support gut health and antibiotics only if inflammation or infection arises.
Managing Diverticulitis: Medications and Procedures
Managing diverticulitis involves the use of antibiotics such as ciprofloxacin and metronidazole to treat infection and reduce inflammation. In severe cases, hospitalization may be required for intravenous antibiotics and fluid therapy to prevent complications. Surgical interventions like bowel resection or drainage of abscesses are considered when conservative treatments fail or complications like perforation or fistulas develop.
Diet and Lifestyle Modifications
Diverticulosis management emphasizes a high-fiber diet rich in fruits, vegetables, and whole grains to promote regular bowel movements and prevent diverticula formation. In contrast, diverticulitis requires temporary dietary adjustments such as low-fiber or clear liquid diets during flare-ups to reduce colon irritation while gradually reintroducing fiber as symptoms improve. Consistent physical activity, adequate hydration, and avoiding smoking play crucial roles in reducing complications and supporting overall digestive health in both conditions.
Potential Complications and Prevention
Diverticulosis can lead to complications such as diverticular bleeding or progression to diverticulitis, which involves inflammation or infection of the diverticula. Diverticulitis may cause abscesses, perforation, peritonitis, or bowel obstruction if untreated. Preventive measures include a high-fiber diet, regular exercise, adequate hydration, and avoiding smoking to reduce the risk of diverticula formation and inflammation.
When to Seek Medical Attention
Seek medical attention for diverticulitis if you experience severe abdominal pain, fever, nausea, or persistent changes in bowel habits, as these symptoms indicate inflammation or infection. Diverticulosis often remains symptom-free and does not usually require urgent care, but sudden intense pain or rectal bleeding should prompt immediate medical evaluation. Early diagnosis and treatment are crucial to prevent complications such as abscess, perforation, or bowel obstruction associated with diverticulitis.
Diverticulosis vs Diverticulitis Infographic
 difterm.com
difterm.com