Rehydration therapy primarily targets the restoration of lost fluids and essential electrolytes to treat dehydration in pets, promoting rapid recovery and maintaining cellular functions. Fluid replacement therapy involves administering intravenous or subcutaneous fluids to address severe dehydration or imbalances caused by illness, injury, or surgery. Both therapies are crucial in veterinary care but differ in their delivery methods and severity of conditions treated.
Table of Comparison
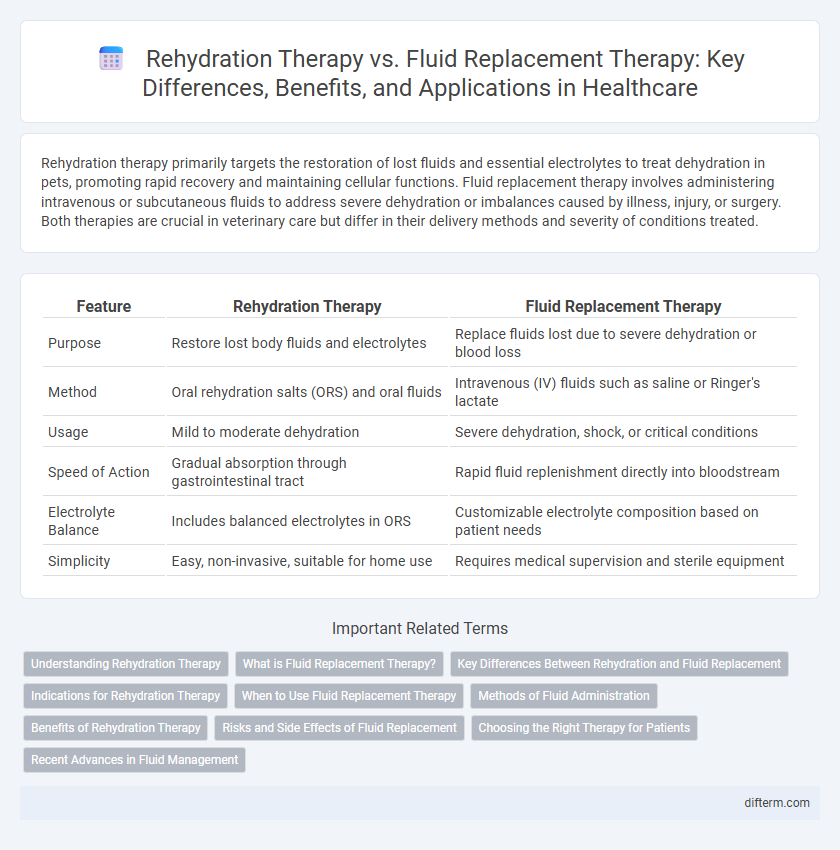
| Feature | Rehydration Therapy | Fluid Replacement Therapy |
|---|---|---|
| Purpose | Restore lost body fluids and electrolytes | Replace fluids lost due to severe dehydration or blood loss |
| Method | Oral rehydration salts (ORS) and oral fluids | Intravenous (IV) fluids such as saline or Ringer's lactate |
| Usage | Mild to moderate dehydration | Severe dehydration, shock, or critical conditions |
| Speed of Action | Gradual absorption through gastrointestinal tract | Rapid fluid replenishment directly into bloodstream |
| Electrolyte Balance | Includes balanced electrolytes in ORS | Customizable electrolyte composition based on patient needs |
| Simplicity | Easy, non-invasive, suitable for home use | Requires medical supervision and sterile equipment |
Understanding Rehydration Therapy
Rehydration therapy focuses specifically on restoring lost fluids and electrolytes caused by dehydration, often through oral rehydration solutions (ORS) containing balanced salts and glucose to enhance absorption. This therapy is critical in treating conditions like diarrhea, heat exhaustion, and mild to moderate dehydration, aiming to quickly reestablish cellular hydration and electrolyte balance. Unlike general fluid replacement therapy, which may involve intravenous administration of fluids for diverse medical conditions, rehydration therapy emphasizes restoring optimal hydration using precise electrolyte formulations.
What is Fluid Replacement Therapy?
Fluid replacement therapy involves the administration of intravenous or oral fluids to restore the body's fluid balance, often used to treat dehydration caused by illness, injury, or surgery. It replaces lost electrolytes and fluids essential for maintaining blood pressure, cellular function, and overall homeostasis. This therapy is critical in managing severe dehydration, shock, and conditions like burns or excessive fluid loss.
Key Differences Between Rehydration and Fluid Replacement
Rehydration therapy primarily targets the restoration of lost electrolytes and water balance caused by dehydration, especially in cases such as diarrhea or heat exhaustion, emphasizing oral or intravenous administration of balanced electrolyte solutions. Fluid replacement therapy involves the wider process of replenishing fluids lost due to blood loss, burns, or surgery, incorporating not only water and electrolytes but also blood products and plasma expanders to maintain circulatory volume and tissue perfusion. The key difference lies in rehydration therapy's focus on correcting electrolyte deficiencies specifically, while fluid replacement therapy addresses comprehensive volume restoration required in critical care scenarios.
Indications for Rehydration Therapy
Rehydration therapy is primarily indicated for treating dehydration caused by conditions such as diarrhea, vomiting, or excessive sweating, where there is significant loss of electrolytes and fluids. It is essential in managing mild to moderate dehydration, especially in pediatric and elderly populations, to restore electrolyte balance and prevent complications. Unlike general fluid replacement therapy, rehydration therapy specifically targets rapid fluid and electrolyte replenishment to maintain cellular function and physiological homeostasis.
When to Use Fluid Replacement Therapy
Fluid replacement therapy is essential in cases of severe dehydration caused by significant fluid loss from conditions such as hemorrhage, burns, or extensive diarrhea. It is prioritized when rapid restoration of blood volume and electrolyte balance is critical to prevent hypovolemic shock and organ failure. Unlike oral rehydration therapy, fluid replacement therapy is typically administered intravenously to ensure immediate absorption and effectiveness in emergency medical situations.
Methods of Fluid Administration
Rehydration therapy primarily employs oral rehydration solutions (ORS) to restore electrolyte balance and hydration through gastrointestinal absorption, often preferred for mild to moderate dehydration. Fluid replacement therapy typically involves intravenous (IV) administration of fluids such as isotonic saline or lactated Ringer's solution, ensuring rapid and controlled volume restoration in severe dehydration or shock. Both methods prioritize maintaining electrolyte stability but differ significantly in administration routes and clinical settings.
Benefits of Rehydration Therapy
Rehydration therapy efficiently restores electrolytes and fluid balance in patients suffering from dehydration, particularly in cases of diarrhea or heat exhaustion. It reduces the risk of complications like kidney failure and shock by promoting rapid absorption of fluids via oral or intravenous routes. The therapy's targeted approach supports quicker recovery and improves overall patient outcomes compared to general fluid replacement methods.
Risks and Side Effects of Fluid Replacement
Fluid replacement therapy carries risks such as fluid overload, which can lead to pulmonary edema and heart failure, especially in patients with compromised cardiac or renal function. Electrolyte imbalances, including hypernatremia or hyponatremia, may occur if fluids are not carefully monitored and adjusted according to individual patient needs. Infection risk is also a concern when intravenous catheters are used for fluid administration, potentially leading to sepsis if aseptic techniques are not strictly followed.
Choosing the Right Therapy for Patients
Rehydration therapy primarily targets electrolyte balance restoration using oral rehydration solutions, making it ideal for mild to moderate dehydration cases, especially in gastroenteritis patients. Fluid replacement therapy involves intravenous administration of fluids, suitable for severe dehydration or when oral intake is not feasible, ensuring rapid circulatory volume restoration. Clinicians must evaluate dehydration severity, patient hydration status, and underlying conditions to determine the appropriate therapy for optimal recovery.
Recent Advances in Fluid Management
Recent advances in fluid management emphasize the differentiation between rehydration therapy and fluid replacement therapy, where rehydration therapy targets extracellular fluid restoration primarily in dehydration cases through oral rehydration solutions optimized for electrolyte balance. Fluid replacement therapy is critical in managing hypovolemia and shock, utilizing intravenous isotonic crystalloids or colloids tailored to restore intravascular volume rapidly. Innovations include the development of balanced electrolyte solutions and goal-directed fluid therapy protocols enhancing patient outcomes in critical care settings.
Rehydration therapy vs Fluid replacement therapy Infographic
 difterm.com
difterm.com