Hypothyroidism in pets is characterized by clear clinical symptoms such as lethargy, weight gain, and hair loss due to insufficient thyroid hormone production. Subclinical hypothyroidism, however, presents with normal or mildly altered thyroid hormone levels without obvious symptoms, making it challenging to detect without laboratory testing. Accurate diagnosis is essential to differentiate between the two conditions and to implement appropriate treatment strategies for optimal pet health.
Table of Comparison
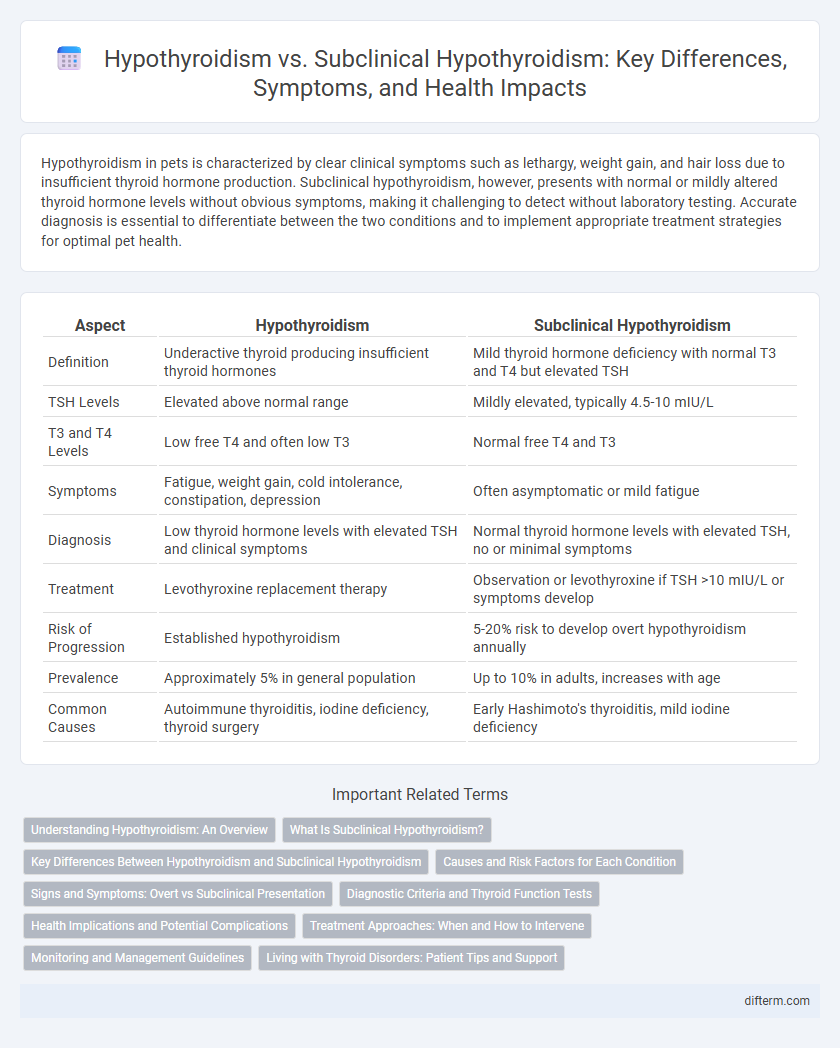
| Aspect | Hypothyroidism | Subclinical Hypothyroidism |
|---|---|---|
| Definition | Underactive thyroid producing insufficient thyroid hormones | Mild thyroid hormone deficiency with normal T3 and T4 but elevated TSH |
| TSH Levels | Elevated above normal range | Mildly elevated, typically 4.5-10 mIU/L |
| T3 and T4 Levels | Low free T4 and often low T3 | Normal free T4 and T3 |
| Symptoms | Fatigue, weight gain, cold intolerance, constipation, depression | Often asymptomatic or mild fatigue |
| Diagnosis | Low thyroid hormone levels with elevated TSH and clinical symptoms | Normal thyroid hormone levels with elevated TSH, no or minimal symptoms |
| Treatment | Levothyroxine replacement therapy | Observation or levothyroxine if TSH >10 mIU/L or symptoms develop |
| Risk of Progression | Established hypothyroidism | 5-20% risk to develop overt hypothyroidism annually |
| Prevalence | Approximately 5% in general population | Up to 10% in adults, increases with age |
| Common Causes | Autoimmune thyroiditis, iodine deficiency, thyroid surgery | Early Hashimoto's thyroiditis, mild iodine deficiency |
Understanding Hypothyroidism: An Overview
Hypothyroidism is a condition characterized by insufficient thyroid hormone production, leading to symptoms like fatigue, weight gain, and depression, while subclinical hypothyroidism presents with mildly elevated thyroid-stimulating hormone (TSH) levels but normal free thyroid hormones, often without noticeable symptoms. Diagnosis involves blood tests measuring TSH and free T4 levels, with subclinical hypothyroidism requiring careful monitoring due to its potential progression to overt hypothyroidism. Effective management of hypothyroidism typically includes levothyroxine therapy to restore normal hormone levels, whereas treatment decisions for subclinical hypothyroidism depend on factors such as TSH concentrations, patient symptoms, and risk of cardiovascular disease.
What Is Subclinical Hypothyroidism?
Subclinical hypothyroidism is a mild form of hypothyroidism where thyroid-stimulating hormone (TSH) levels are elevated, but free thyroxine (T4) levels remain within the normal range. This condition often presents with minimal or no obvious symptoms, making it detectable primarily through blood tests. It differs from overt hypothyroidism, which is characterized by both elevated TSH and low T4 levels, leading to more pronounced clinical manifestations.
Key Differences Between Hypothyroidism and Subclinical Hypothyroidism
Hypothyroidism is characterized by low thyroid hormone levels and overt symptoms such as fatigue, weight gain, and cold intolerance, while subclinical hypothyroidism presents with elevated thyroid-stimulating hormone (TSH) but normal free thyroxine (T4) levels, often lacking noticeable symptoms. Diagnosis of hypothyroidism involves clearly abnormal thyroid function tests, whereas subclinical hypothyroidism is identified primarily through biochemical markers without significant clinical manifestations. Treatment typically starts immediately for hypothyroidism due to symptomatic hormone deficiency, while subclinical hypothyroidism management depends on factors like TSH levels, presence of symptoms, and risk of progression to overt disease.
Causes and Risk Factors for Each Condition
Hypothyroidism is primarily caused by autoimmune thyroiditis, iodine deficiency, and thyroid surgery, leading to significantly reduced thyroid hormone production. Subclinical hypothyroidism often arises from mild thyroid gland dysfunction, frequently linked to autoimmune thyroiditis or iodine imbalance, but with normal thyroid hormone levels and elevated TSH. Risk factors for both conditions include female gender, age over 60, family history of thyroid disease, and exposure to radiation or certain medications.
Signs and Symptoms: Overt vs Subclinical Presentation
Hypothyroidism presents with clear signs such as fatigue, weight gain, cold intolerance, dry skin, and constipation, reflecting significant thyroid hormone deficiency. Subclinical hypothyroidism typically shows mild or no symptoms, with normal free T4 levels but elevated thyroid-stimulating hormone (TSH), indicating early thyroid dysfunction. Distinguishing between overt and subclinical hypothyroidism is crucial for timely diagnosis and management to prevent progression and complications.
Diagnostic Criteria and Thyroid Function Tests
Hypothyroidism is diagnosed by elevated thyroid-stimulating hormone (TSH) levels above 10 mIU/L combined with low free thyroxine (FT4) levels, whereas subclinical hypothyroidism presents with mildly elevated TSH levels typically between 4.5 and 10 mIU/L and normal FT4 concentrations. Thyroid function tests are essential in differentiating these conditions, with TSH being the most sensitive marker for thyroid dysfunction. Accurate interpretation of TSH and FT4 values guides clinical decisions and management strategies for both overt and subclinical hypothyroidism.
Health Implications and Potential Complications
Hypothyroidism causes overt symptoms such as fatigue, weight gain, and cold intolerance due to insufficient thyroid hormone production, significantly impacting metabolic and cardiovascular health. Subclinical hypothyroidism presents with elevated thyroid-stimulating hormone (TSH) levels but normal thyroid hormones, often remaining asymptomatic yet increasing the risk of progression to overt hypothyroidism and cardiovascular disease. Early diagnosis and management are crucial to preventing complications such as myxedema, infertility, and dyslipidemia associated with untreated hypothyroid conditions.
Treatment Approaches: When and How to Intervene
Treatment approaches for hypothyroidism typically involve daily levothyroxine therapy to normalize thyroid hormone levels and alleviate symptoms, with dosage tailored to individual patient needs based on TSH and free T4 values. Subclinical hypothyroidism intervention is more nuanced, often reserved for patients with TSH levels above 10 mIU/L, presence of thyroid antibodies, symptomatic cases, or those at risk for cardiovascular disease, where low-dose levothyroxine can be considered. Regular monitoring of thyroid function tests every 6 to 12 months is essential in subclinical cases to determine the necessity for initiation or adjustment of therapy.
Monitoring and Management Guidelines
Hypothyroidism requires consistent monitoring of thyroid-stimulating hormone (TSH) and free thyroxine (FT4) levels to adjust levothyroxine therapy, with guidelines recommending follow-up every 6-12 weeks initially and then annually once stable. Subclinical hypothyroidism management depends on TSH levels, patient age, and presence of symptoms or comorbidities, with repeat thyroid function tests advised every 6-12 months if treatment is deferred. Clinical guidelines emphasize individualized care, considering cardiovascular risk factors and symptom progression to decide between active surveillance and initiating hormone replacement.
Living with Thyroid Disorders: Patient Tips and Support
Managing hypothyroidism and subclinical hypothyroidism requires regular monitoring of thyroid hormone levels, adherence to prescribed levothyroxine therapy, and mindful symptom tracking to prevent complications like fatigue and cognitive impairment. Patients benefit from a balanced diet rich in iodine, selenium, and zinc to support thyroid function, while avoiding excessive soy and high-fiber foods that can interfere with medication absorption. Joining thyroid support groups and consulting endocrinologists for personalized care plans enhance mental well-being and treatment adherence in living with thyroid disorders.
Hypothyroidism vs Subclinical Hypothyroidism Infographic
 difterm.com
difterm.com