Continuous Glucose Monitoring (CGM) provides real-time blood sugar data through a sensor, allowing for more accurate and frequent glucose monitoring compared to traditional fingerstick glucose tests. Unlike fingerstick methods that require manual sampling multiple times a day, CGM offers continuous insights and trends, helping to detect fluctuations and prevent hypoglycemia or hyperglycemia. CGM technology enhances diabetes management by enabling proactive adjustments to diet, medication, and lifestyle for better glucose control.
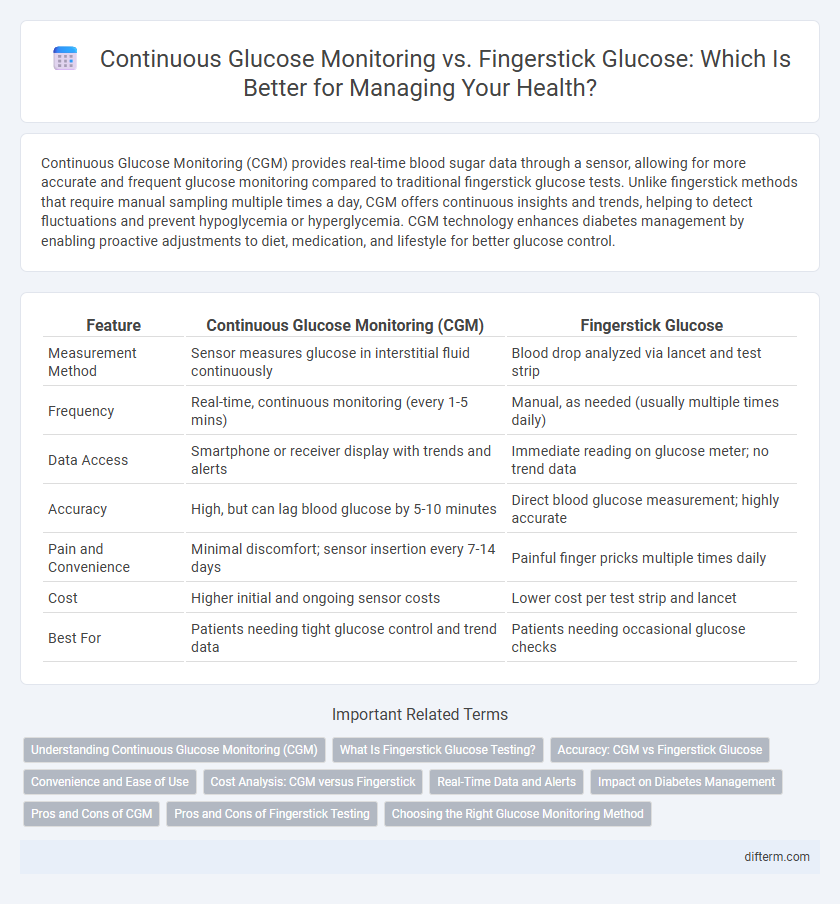
Table of Comparison
| Feature | Continuous Glucose Monitoring (CGM) | Fingerstick Glucose |
|---|---|---|
| Measurement Method | Sensor measures glucose in interstitial fluid continuously | Blood drop analyzed via lancet and test strip |
| Frequency | Real-time, continuous monitoring (every 1-5 mins) | Manual, as needed (usually multiple times daily) |
| Data Access | Smartphone or receiver display with trends and alerts | Immediate reading on glucose meter; no trend data |
| Accuracy | High, but can lag blood glucose by 5-10 minutes | Direct blood glucose measurement; highly accurate |
| Pain and Convenience | Minimal discomfort; sensor insertion every 7-14 days | Painful finger pricks multiple times daily |
| Cost | Higher initial and ongoing sensor costs | Lower cost per test strip and lancet |
| Best For | Patients needing tight glucose control and trend data | Patients needing occasional glucose checks |
Understanding Continuous Glucose Monitoring (CGM)
Continuous Glucose Monitoring (CGM) provides real-time glucose readings through a sensor placed under the skin, offering continuous data that helps in better managing blood sugar levels compared to periodic fingerstick glucose tests. CGM devices track glucose trends and patterns throughout the day and night, enabling timely adjustments in diet, activity, and medication. This technology enhances diabetes care by reducing hypoglycemia risk and improving overall glucose control.
What Is Fingerstick Glucose Testing?
Fingerstick glucose testing involves pricking the finger to obtain a small blood sample for measuring blood sugar levels using a glucose meter. This traditional method provides instant glucose readings but requires multiple daily tests and can cause discomfort due to repeated finger pricking. It remains a widely used, cost-effective approach for routine blood glucose monitoring in diabetes management.
Accuracy: CGM vs Fingerstick Glucose
Continuous Glucose Monitoring (CGM) provides real-time glucose data with minimal lag, offering more comprehensive trends compared to periodic fingerstick glucose measurements. Fingerstick glucose testing delivers point-in-time accuracy using capillary blood samples but may miss fluctuations occurring between tests. Studies show CGM systems have comparable accuracy to fingerstick devices, with the added benefit of continuous data aiding in better glucose management and timely interventions.
Convenience and Ease of Use
Continuous Glucose Monitoring (CGM) offers significant convenience by providing real-time glucose data through a sensor worn on the skin, eliminating the need for frequent fingerstick tests. Unlike fingerstick glucose monitoring, which requires multiple daily blood samples and manual logging, CGM systems automatically track glucose trends and alert users to hypo- or hyperglycemia. This hands-free approach enhances ease of use, especially for individuals managing diabetes who benefit from continuous, hassle-free glucose insights.
Cost Analysis: CGM versus Fingerstick
Continuous Glucose Monitoring (CGM) systems typically incur higher initial costs due to sensor and transmitter expenses, averaging $2,500 to $6,000 annually, compared to fingerstick glucose meters whose strips cost about $1 to $1.50 each, totaling approximately $500 to $1,200 yearly based on usage frequency. While CGM offers real-time glucose readings and reduces long-term complications by improving glycemic control, the upfront investment can be a barrier for many patients without insurance coverage. Cost-effectiveness analyses suggest that CGM may lead to lower healthcare costs over time by preventing diabetes-related hospitalizations and complications, making it a valuable tool despite higher immediate expenses.
Real-Time Data and Alerts
Continuous Glucose Monitoring (CGM) provides real-time glucose data, enabling immediate detection of blood sugar fluctuations through constant sensor readings. Unlike fingerstick glucose testing, which offers only periodic snapshots, CGM systems deliver continuous alerts for hypo- or hyperglycemia, improving proactive diabetes management. Real-time data from CGM enhances patient safety by reducing the risk of unnoticed glucose extremes and enabling timely interventions.
Impact on Diabetes Management
Continuous Glucose Monitoring (CGM) significantly enhances diabetes management by providing real-time glucose trends, allowing for timely insulin adjustments that reduce hypoglycemic events. Fingerstick glucose testing offers discrete, intermittent data points but lacks the comprehensive glucose pattern insights essential for proactive decision-making. Studies show CGM use lowers HbA1c levels and improves overall glycemic control compared to traditional fingerstick methods.
Pros and Cons of CGM
Continuous Glucose Monitoring (CGM) offers real-time glucose data, enabling better glycemic control and reducing hypoglycemia risk compared to traditional fingerstick glucose monitoring. However, CGM devices can be costly, require sensor replacement every 7-14 days, and may cause skin irritation for some users. Despite these drawbacks, CGM improves diabetes management by providing continuous insights that fingerstick tests cannot capture.
Pros and Cons of Fingerstick Testing
Fingerstick glucose testing offers quick and cost-effective blood sugar monitoring, requiring minimal equipment and providing reliable spot-check results for diabetes management. However, it involves frequent finger pricks that can cause discomfort, has limited data since it captures glucose levels only at specific moments, and lacks the real-time trend information provided by continuous glucose monitoring (CGM) devices. Despite these drawbacks, fingerstick testing remains widely used due to its accessibility and insurance coverage.
Choosing the Right Glucose Monitoring Method
Continuous Glucose Monitoring (CGM) provides real-time glucose level tracking through a sensor, allowing for timely adjustments in diabetes management, while fingerstick glucose testing offers intermittent, point-in-time measurements using blood samples. CGM is preferable for individuals requiring dynamic, comprehensive glucose data to detect trends and prevent hypoglycemia, whereas fingerstick monitoring remains suitable for those needing cost-effective, straightforward checks. Selecting the appropriate method depends on factors such as lifestyle, budget, diabetes type, and the need for detailed glucose insights.
Continuous Glucose Monitoring vs Fingerstick Glucose Infographic
 difterm.com
difterm.com