Cushing's syndrome results from excessive cortisol production, causing symptoms like weight gain, high blood pressure, and muscle weakness. Addison's disease is characterized by insufficient cortisol and often aldosterone, leading to fatigue, weight loss, and low blood pressure. Both disorders affect adrenal gland function but require distinct diagnostic approaches and treatments.
Table of Comparison
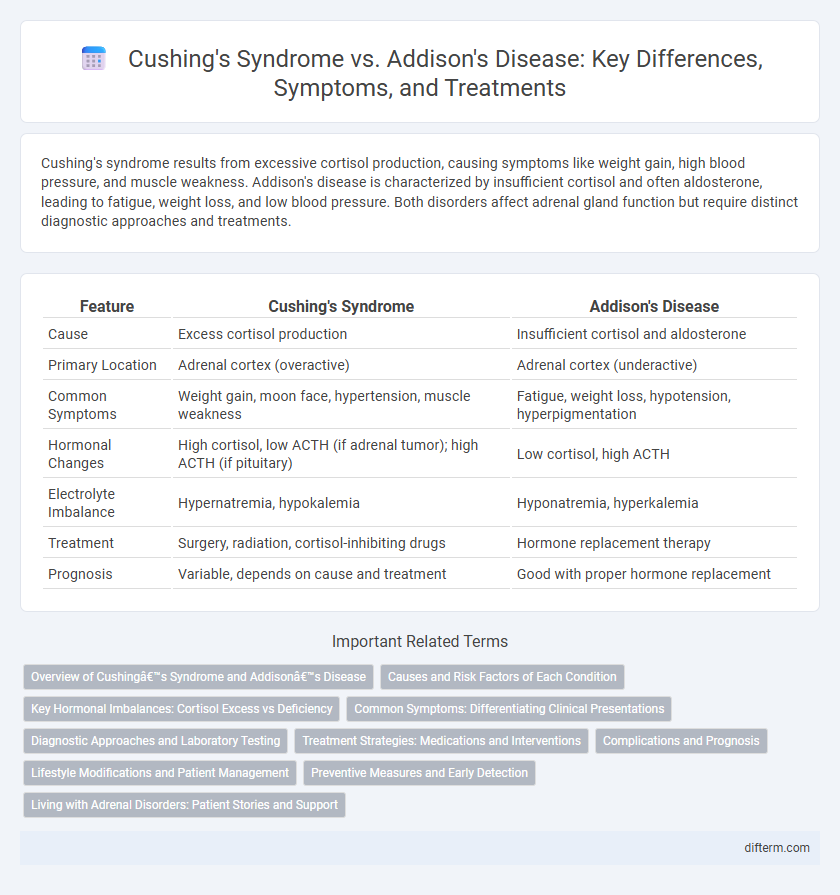
| Feature | Cushing's Syndrome | Addison's Disease |
|---|---|---|
| Cause | Excess cortisol production | Insufficient cortisol and aldosterone |
| Primary Location | Adrenal cortex (overactive) | Adrenal cortex (underactive) |
| Common Symptoms | Weight gain, moon face, hypertension, muscle weakness | Fatigue, weight loss, hypotension, hyperpigmentation |
| Hormonal Changes | High cortisol, low ACTH (if adrenal tumor); high ACTH (if pituitary) | Low cortisol, high ACTH |
| Electrolyte Imbalance | Hypernatremia, hypokalemia | Hyponatremia, hyperkalemia |
| Treatment | Surgery, radiation, cortisol-inhibiting drugs | Hormone replacement therapy |
| Prognosis | Variable, depends on cause and treatment | Good with proper hormone replacement |
Overview of Cushing’s Syndrome and Addison’s Disease
Cushing's syndrome results from prolonged exposure to high cortisol levels, often caused by adrenal tumors or long-term steroid use, leading to symptoms such as weight gain, hypertension, and muscle weakness. Addison's disease is characterized by insufficient production of cortisol and aldosterone due to adrenal gland destruction or dysfunction, causing symptoms like fatigue, weight loss, low blood pressure, and hyperpigmentation. Both conditions involve adrenal hormone imbalances but differ significantly in their pathophysiology, clinical presentation, and treatment approaches.
Causes and Risk Factors of Each Condition
Cushing's syndrome is primarily caused by prolonged exposure to high cortisol levels, often due to corticosteroid medications or adrenal gland tumors, with risk factors including chronic stress and pituitary adenomas. Addison's disease results from adrenal insufficiency, frequently caused by autoimmune destruction of the adrenal cortex or infections like tuberculosis, with risk factors encompassing genetic predisposition and other autoimmune disorders. Understanding the distinct etiologies aids in accurate diagnosis and targeted treatment strategies for these endocrine conditions.
Key Hormonal Imbalances: Cortisol Excess vs Deficiency
Cushing's syndrome is characterized by cortisol excess due to overproduction by the adrenal glands or prolonged glucocorticoid therapy, resulting in symptoms like weight gain, hypertension, and hyperglycemia. Addison's disease involves cortisol deficiency caused by adrenal insufficiency, leading to fatigue, hypotension, and hyperpigmentation. Both conditions highlight the critical role of cortisol in maintaining metabolic and immune system balance.
Common Symptoms: Differentiating Clinical Presentations
Cushing's syndrome commonly presents with symptoms such as central obesity, moon face, hypertension, and purple striae, reflecting cortisol excess. In contrast, Addison's disease is characterized by fatigue, weight loss, hyperpigmentation, and hypotension due to adrenal insufficiency. Understanding these distinct clinical features aids in the accurate differentiation and diagnosis of adrenal gland disorders.
Diagnostic Approaches and Laboratory Testing
Diagnostic approaches for Cushing's syndrome primarily involve measuring elevated cortisol levels through 24-hour urinary free cortisol tests, low-dose dexamethasone suppression tests, and late-night salivary cortisol assays. Addison's disease diagnosis relies on detecting insufficient cortisol and aldosterone using serum cortisol measurements, adrenocorticotropic hormone (ACTH) stimulation tests, and electrolyte panels showing hyponatremia and hyperkalemia. Imaging studies such as adrenal CT scans supplement laboratory findings to differentiate adrenal causes in both disorders.
Treatment Strategies: Medications and Interventions
Treatment strategies for Cushing's syndrome often involve medications such as ketoconazole or metyrapone to inhibit cortisol production, alongside surgical removal of adrenal or pituitary tumors when necessary. Addison's disease requires lifelong hormone replacement therapy, including glucocorticoids like hydrocortisone and mineralocorticoids such as fludrocortisone to maintain electrolyte balance and support adrenal function. Both conditions demand careful monitoring and individualized intervention plans to optimize patient outcomes and manage hormone levels effectively.
Complications and Prognosis
Cushing's syndrome, caused by prolonged exposure to high cortisol levels, can lead to complications such as hypertension, diabetes mellitus, osteoporosis, and increased risk of cardiovascular disease, significantly impacting long-term prognosis without appropriate treatment. Addison's disease, characterized by adrenal insufficiency and low cortisol production, often results in chronic fatigue, hypotension, electrolyte imbalances, and can cause life-threatening adrenal crisis if untreated, making early diagnosis and hormone replacement critical for improved outcomes. Prognosis for both conditions depends on timely management and addressing underlying causes, with untreated Cushing's syndrome leading to severe metabolic disturbances and Addison's disease requiring lifelong glucocorticoid therapy to prevent morbidity and mortality.
Lifestyle Modifications and Patient Management
Effective lifestyle modifications for Cushing's syndrome include adopting a balanced diet low in sodium and high in potassium to manage blood pressure and reduce fluid retention, while regular physical activity helps improve muscle strength and bone density affected by excess cortisol. Addison's disease management emphasizes consistent cortisol replacement therapy, maintaining adequate salt intake, and stress management techniques to prevent adrenal crises. Both conditions require regular medical monitoring and patient education to recognize symptoms early and adjust treatment accordingly.
Preventive Measures and Early Detection
Preventive measures for Cushing's syndrome and Addison's disease emphasize regular medical check-ups and monitoring adrenal function in at-risk populations, such as those on prolonged corticosteroid therapy. Early detection relies heavily on blood tests measuring cortisol and ACTH levels, alongside imaging studies like MRI or CT scans to assess adrenal or pituitary abnormalities. Timely identification through these diagnostic tools significantly improves treatment outcomes and reduces complications associated with hormonal imbalances.
Living with Adrenal Disorders: Patient Stories and Support
Living with adrenal disorders such as Cushing's syndrome and Addison's disease presents unique daily challenges, including managing hormone imbalances and coping with fluctuating energy levels. Patient stories highlight the importance of tailored treatment plans, regular endocrinologist consultations, and access to mental health support to improve quality of life. Support groups and online communities provide valuable resources and emotional support, helping individuals share experiences and strategies for navigating these chronic conditions.
Cushing’s syndrome vs Addison’s disease Infographic
 difterm.com
difterm.com