Obstructive sleep apnea occurs when the throat muscles intermittently relax and block the airway during sleep, causing breathing pauses. Central sleep apnea involves the brain failing to send proper signals to the muscles that control breathing, resulting in disrupted respiratory effort. Differentiating between these types is crucial for effective treatment, as obstructive sleep apnea often benefits from airway support devices while central sleep apnea may require addressing underlying neurological or cardiac conditions.
Table of Comparison
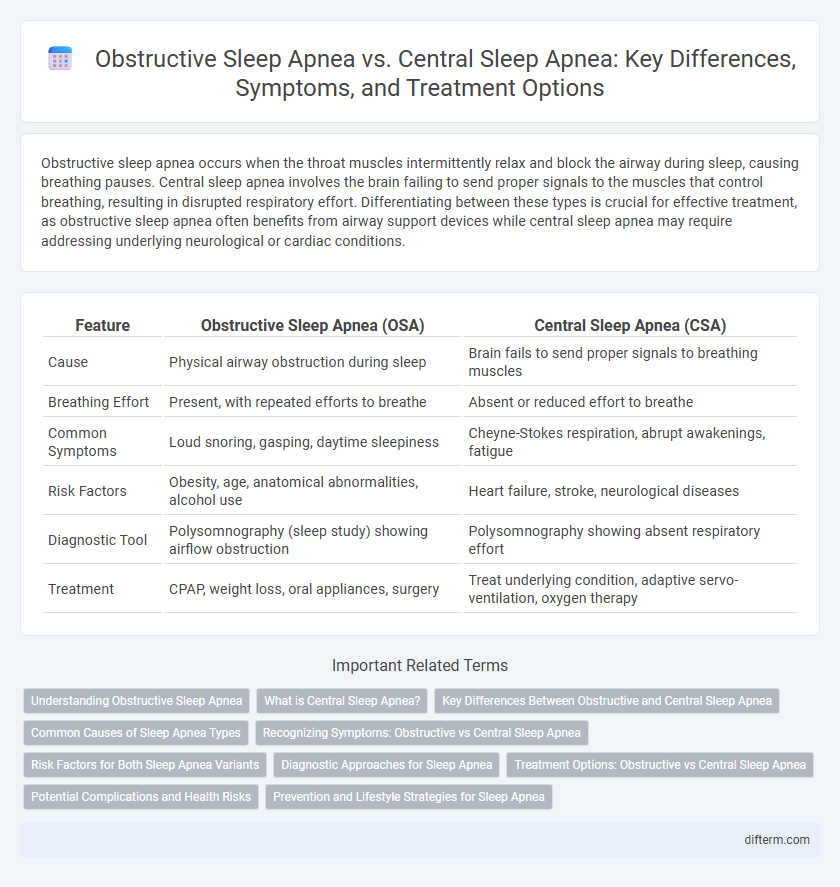
| Feature | Obstructive Sleep Apnea (OSA) | Central Sleep Apnea (CSA) |
|---|---|---|
| Cause | Physical airway obstruction during sleep | Brain fails to send proper signals to breathing muscles |
| Breathing Effort | Present, with repeated efforts to breathe | Absent or reduced effort to breathe |
| Common Symptoms | Loud snoring, gasping, daytime sleepiness | Cheyne-Stokes respiration, abrupt awakenings, fatigue |
| Risk Factors | Obesity, age, anatomical abnormalities, alcohol use | Heart failure, stroke, neurological diseases |
| Diagnostic Tool | Polysomnography (sleep study) showing airflow obstruction | Polysomnography showing absent respiratory effort |
| Treatment | CPAP, weight loss, oral appliances, surgery | Treat underlying condition, adaptive servo-ventilation, oxygen therapy |
Understanding Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) is a common sleep disorder characterized by repeated upper airway blockages during sleep, leading to interrupted breathing and reduced oxygen levels. Unlike central sleep apnea, which involves a lack of respiratory effort due to brain signaling issues, OSA is primarily caused by physical obstruction of the airway, often related to excess tissue or relaxed throat muscles. Understanding the anatomy and risk factors of OSA, such as obesity, age, and neck circumference, is crucial for effective diagnosis and treatment.
What is Central Sleep Apnea?
Central sleep apnea (CSA) is a sleep disorder characterized by repeated pauses in breathing due to the brain's failure to send proper signals to the muscles that control respiration. Unlike obstructive sleep apnea (OSA), which results from a physical blockage of the airway, CSA involves a disconnect in the neurological control of breathing. This condition often occurs in individuals with heart failure, stroke, or certain neurological disorders and requires specialized diagnosis and treatment to manage the underlying causes effectively.
Key Differences Between Obstructive and Central Sleep Apnea
Obstructive sleep apnea (OSA) occurs due to physical blockage of the airway, causing interrupted breathing despite ongoing respiratory effort, whereas central sleep apnea (CSA) results from the brain's failure to send proper signals to the muscles controlling breathing. OSA is commonly linked to obesity, snoring, and airway anatomy abnormalities, while CSA often associates with neurological disorders, heart failure, or opioid use. Diagnostic tools like polysomnography reveal distinctive patterns: OSA shows continued respiratory effort with airflow obstruction, whereas CSA exhibits a complete absence of respiratory effort during apnea episodes.
Common Causes of Sleep Apnea Types
Obstructive sleep apnea (OSA) commonly results from physical blockages like enlarged tonsils, obesity, or anatomical abnormalities that restrict airflow during sleep. Central sleep apnea (CSA) primarily arises from neurological issues such as heart failure, stroke, or damage to the brainstem that disrupt respiratory control. Understanding these distinct causes aids in accurate diagnosis and targeted treatment strategies for effective management of each sleep apnea type.
Recognizing Symptoms: Obstructive vs Central Sleep Apnea
Obstructive sleep apnea (OSA) often presents with loud snoring, gasping, and frequent awakenings due to airway blockage, while central sleep apnea (CSA) is characterized by pauses in breathing caused by the brain's failure to send proper signals to the muscles controlling respiration. Individuals with OSA may experience excessive daytime sleepiness and morning headaches, contrasting with CSA symptoms that include irregular breathing patterns and abrupt awakenings without airway obstruction. Accurate symptom recognition is essential for diagnosis, as OSA is linked to anatomical airway issues, whereas CSA typically involves neurological or cardiac conditions.
Risk Factors for Both Sleep Apnea Variants
Obstructive sleep apnea (OSA) risk factors include obesity, neck circumference over 17 inches, male gender, and anatomical abnormalities such as a deviated septum or enlarged tonsils. Central sleep apnea (CSA) risk factors primarily involve underlying medical conditions like heart failure, stroke, and opioid use, as well as high-altitude exposure. Both OSA and CSA share risk factors such as advanced age, male gender, and the presence of comorbid conditions like hypertension and diabetes.
Diagnostic Approaches for Sleep Apnea
Diagnostic approaches for obstructive sleep apnea (OSA) primarily involve polysomnography, which monitors breathing patterns, oxygen levels, and airway obstructions during sleep. Central sleep apnea (CSA) is diagnosed using similar sleep studies but focuses on identifying irregularities in respiratory effort and neurologic control of breathing. Advanced techniques such as home sleep apnea testing and capnography can aid in differentiating between OSA and CSA to tailor appropriate treatment strategies.
Treatment Options: Obstructive vs Central Sleep Apnea
Treatment for obstructive sleep apnea primarily involves continuous positive airway pressure (CPAP) therapy, which keeps the airway open during sleep, along with lifestyle changes such as weight loss and positional therapy. Central sleep apnea treatment focuses on addressing the underlying medical condition, with options including adaptive servo-ventilation (ASV), oxygen therapy, and in some cases, medications like acetazolamide to stimulate breathing. Both types may benefit from sleep hygiene improvements, but specific interventions depend on whether airway obstruction or neurological control of breathing is the root cause.
Potential Complications and Health Risks
Obstructive sleep apnea (OSA) leads to intermittent airway blockage causing oxygen desaturation and increased risk of hypertension, cardiovascular disease, and stroke. Central sleep apnea (CSA) results from brain signal disruptions affecting breathing regulation, elevating the potential for heart failure, arrhythmias, and neurocognitive impairment. Both conditions increase daytime fatigue, impaired concentration, and reduce overall quality of life if left untreated.
Prevention and Lifestyle Strategies for Sleep Apnea
Obstructive sleep apnea prevention centers on maintaining a healthy weight, avoiding alcohol and sedatives before bedtime, and sleeping on one's side to keep the airway open. Central sleep apnea management involves addressing underlying conditions such as heart failure or stroke, minimizing opioid use, and using adaptive servo-ventilation devices when prescribed. Both disorders benefit from lifestyle changes like regular exercise, good sleep hygiene, and quitting smoking to reduce symptoms and improve overall sleep quality.
Obstructive sleep apnea vs central sleep apnea Infographic
 difterm.com
difterm.com