Autoimmunity occurs when the immune system mistakenly attacks the body's own cells, leading to chronic inflammation and tissue damage. Alloimmunity involves an immune response against non-self antigens from another individual of the same species, commonly seen in organ transplantation and blood transfusions. Understanding the differences between autoimmunity and alloimmunity is crucial for developing targeted therapies and improving patient outcomes.
Table of Comparison
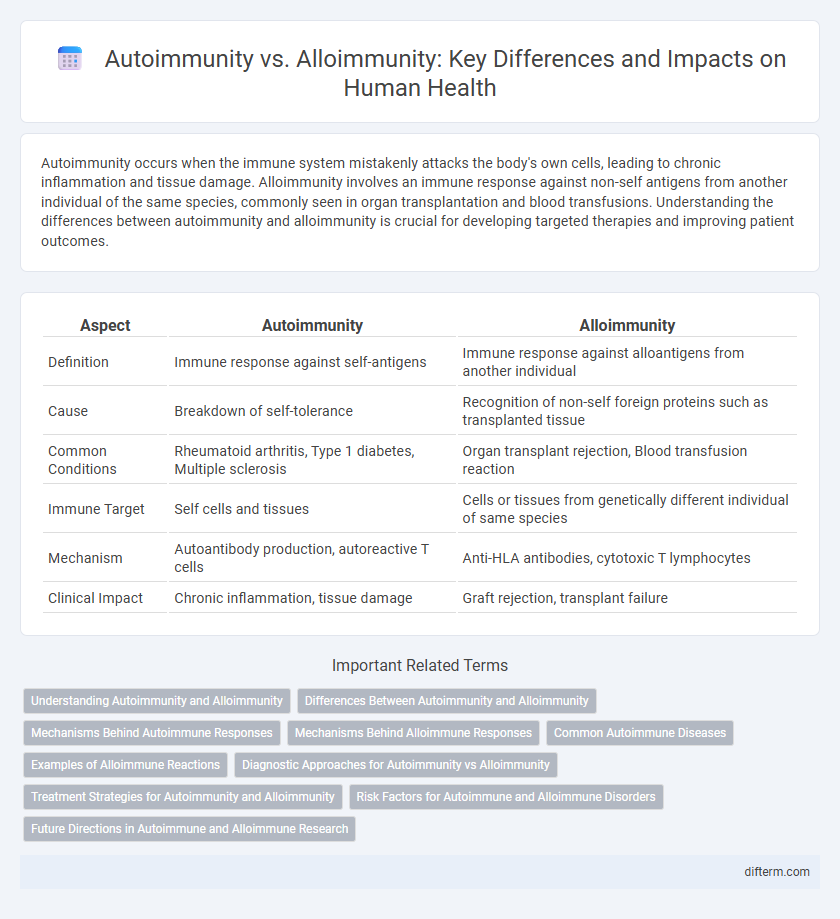
| Aspect | Autoimmunity | Alloimmunity |
|---|---|---|
| Definition | Immune response against self-antigens | Immune response against alloantigens from another individual |
| Cause | Breakdown of self-tolerance | Recognition of non-self foreign proteins such as transplanted tissue |
| Common Conditions | Rheumatoid arthritis, Type 1 diabetes, Multiple sclerosis | Organ transplant rejection, Blood transfusion reaction |
| Immune Target | Self cells and tissues | Cells or tissues from genetically different individual of same species |
| Mechanism | Autoantibody production, autoreactive T cells | Anti-HLA antibodies, cytotoxic T lymphocytes |
| Clinical Impact | Chronic inflammation, tissue damage | Graft rejection, transplant failure |
Understanding Autoimmunity and Alloimmunity
Autoimmunity occurs when the immune system mistakenly targets the body's own tissues, leading to chronic inflammation and tissue damage seen in diseases such as rheumatoid arthritis and type 1 diabetes. Alloimmunity involves immune responses against non-self antigens from the same species, commonly seen in transplant rejection and blood transfusion reactions. Distinguishing the mechanisms and targets of autoimmunity versus alloimmunity is crucial for developing targeted immunotherapies and improving transplant outcomes.
Differences Between Autoimmunity and Alloimmunity
Autoimmunity occurs when the immune system mistakenly targets the body's own tissues, leading to diseases like rheumatoid arthritis and lupus, while alloimmunity involves immune responses against genetically different cells from the same species, such as in organ transplantation or blood transfusion rejection. Autoimmune reactions are triggered by self-antigens, whereas alloimmune responses are driven by foreign antigens present on donor tissues. The distinct mechanisms of antigen recognition and immune activation define the fundamental differences between autoimmunity and alloimmunity in clinical immunology.
Mechanisms Behind Autoimmune Responses
Autoimmune responses arise when the immune system mistakenly targets the body's own tissues due to the breakdown of self-tolerance mechanisms, involving autoreactive T cells and autoantibodies. Central tolerance in the thymus eliminates many self-reactive lymphocytes, but peripheral tolerance defects allow surviving autoreactive cells to activate and proliferate. Molecular mimicry, epitope spreading, and bystander activation further contribute to the development and persistence of autoimmune diseases.
Mechanisms Behind Alloimmune Responses
Alloimmune responses are triggered when the immune system recognizes non-self antigens from genetically different members of the same species, primarily involving T-cell activation and antibody production against donor tissues. The mechanism relies on antigen presentation through major histocompatibility complex (MHC) molecules, leading to cytotoxic T lymphocyte-mediated destruction and complement activation. This immune recognition underpins transplant rejection, graft-versus-host disease, and other complications in organ and tissue transplantation.
Common Autoimmune Diseases
Common autoimmune diseases such as rheumatoid arthritis, type 1 diabetes, and multiple sclerosis result from the immune system mistakenly attacking the body's own tissues, distinguishing them from alloimmunity where immune responses target genetically different cells, such as in organ transplantation. Autoimmune disorders involve autoantibodies and autoreactive T cells that cause chronic inflammation and tissue damage. Understanding the mechanisms behind autoimmunity is critical for developing targeted therapies and improving patient outcomes in diseases like systemic lupus erythematosus and Hashimoto's thyroiditis.
Examples of Alloimmune Reactions
Alloimmune reactions occur when the immune system responds to antigens from the same species but genetically different individuals, as seen in organ transplantation rejection, such as kidney or liver transplants. Another example includes hemolytic disease of the newborn, where maternal antibodies attack fetal red blood cells expressing paternal antigens. Blood transfusion reactions also illustrate alloimmunity, with immune responses triggered against incompatible donor blood group antigens causing hemolysis.
Diagnostic Approaches for Autoimmunity vs Alloimmunity
Diagnostic approaches for autoimmunity primarily involve serological tests detecting autoantibodies such as antinuclear antibodies (ANA) and disease-specific markers like anti-dsDNA for systemic lupus erythematosus. Alloimmunity diagnosis centers on identifying donor-specific antibodies (DSA) through assays like Luminex single-antigen bead testing and crossmatch procedures to assess transplant compatibility. Advanced imaging and biopsy complement these tests to evaluate organ involvement and immune-mediated tissue damage in both autoimmune and alloimmune conditions.
Treatment Strategies for Autoimmunity and Alloimmunity
Treatment strategies for autoimmunity primarily involve immunosuppressive drugs such as corticosteroids, biologics targeting specific immune pathways like TNF inhibitors, and therapies that restore immune tolerance, including regulatory T cell enhancement. Alloimmunity management centers on preventing graft rejection through immunosuppressants like calcineurin inhibitors, antiproliferative agents, and monoclonal antibodies that inhibit T cell activation. Emerging therapies for both conditions explore personalized medicine approaches, immune modulation, and gene editing to improve efficacy and reduce systemic side effects.
Risk Factors for Autoimmune and Alloimmune Disorders
Genetic predisposition, environmental triggers, and hormonal influences are primary risk factors for autoimmune disorders, often leading to the immune system attacking the body's own tissues. Alloimmune disorders, in contrast, arise from immune responses to non-self antigens following organ transplantation or pregnancy, with factors such as donor-recipient HLA mismatch and prior sensitization significantly increasing risk. Understanding these distinct etiologies is crucial for developing targeted prevention and management strategies in immune-mediated diseases.
Future Directions in Autoimmune and Alloimmune Research
Emerging research in autoimmunity and alloimmunity is exploring advanced gene-editing techniques such as CRISPR to modulate immune responses and develop targeted therapies. Biomarker discovery and personalized medicine are driving precision treatment approaches that improve patient outcomes in autoimmune diseases and transplantation compatibility. Innovations in immunomodulatory biologics and tolerance induction strategies hold promise for reducing long-term complications and enhancing graft survival in alloimmunity.
Autoimmunity vs Alloimmunity Infographic
 difterm.com
difterm.com