Orthostatic hypotension occurs when blood pressure drops significantly upon standing, leading to dizziness and potential fainting due to inadequate cerebral blood flow. Postprandial hypotension, on the other hand, happens after eating, as blood is redirected to the digestive system, causing blood pressure to decline and possibly resulting in lightheadedness or falls. Both conditions require monitoring and management to prevent complications, especially in older adults or those with underlying cardiovascular issues.
Table of Comparison
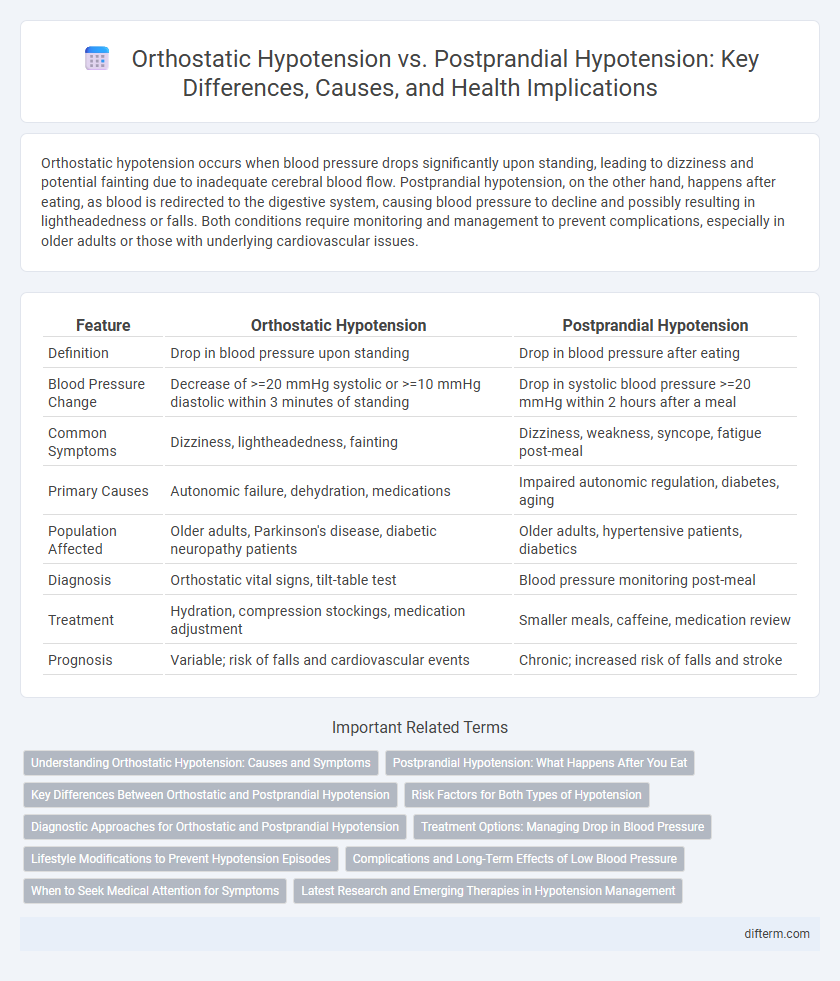
| Feature | Orthostatic Hypotension | Postprandial Hypotension |
|---|---|---|
| Definition | Drop in blood pressure upon standing | Drop in blood pressure after eating |
| Blood Pressure Change | Decrease of >=20 mmHg systolic or >=10 mmHg diastolic within 3 minutes of standing | Drop in systolic blood pressure >=20 mmHg within 2 hours after a meal |
| Common Symptoms | Dizziness, lightheadedness, fainting | Dizziness, weakness, syncope, fatigue post-meal |
| Primary Causes | Autonomic failure, dehydration, medications | Impaired autonomic regulation, diabetes, aging |
| Population Affected | Older adults, Parkinson's disease, diabetic neuropathy patients | Older adults, hypertensive patients, diabetics |
| Diagnosis | Orthostatic vital signs, tilt-table test | Blood pressure monitoring post-meal |
| Treatment | Hydration, compression stockings, medication adjustment | Smaller meals, caffeine, medication review |
| Prognosis | Variable; risk of falls and cardiovascular events | Chronic; increased risk of falls and stroke |
Understanding Orthostatic Hypotension: Causes and Symptoms
Orthostatic hypotension is characterized by a significant drop in blood pressure upon standing, commonly caused by dehydration, prolonged bed rest, or certain medications affecting autonomic nervous system function. Symptoms include dizziness, lightheadedness, blurred vision, and fainting, which occur due to insufficient cerebral blood flow when moving to an upright position. Differentiating it from postprandial hypotension, which happens after meals, is crucial for targeted treatment and management.
Postprandial Hypotension: What Happens After You Eat
Postprandial hypotension causes a significant drop in blood pressure within 30 to 90 minutes after eating, due to blood being diverted to the digestive system. This condition often leads to dizziness, fainting, and falls, particularly in older adults or those with autonomic dysfunction. Managing meal size, composition, and timing is crucial to reducing symptoms and maintaining cardiovascular stability after eating.
Key Differences Between Orthostatic and Postprandial Hypotension
Orthostatic hypotension is characterized by a significant drop in blood pressure upon standing, often defined as a decrease of at least 20 mmHg systolic or 10 mmHg diastolic within three minutes of standing. In contrast, postprandial hypotension occurs within two hours after eating, involving a decrease in systolic blood pressure by 20 mmHg or more due to blood flow shifting to the digestive system. The primary distinction lies in their triggers: orthostatic hypotension results from positional changes, while postprandial hypotension is meal-induced, affecting blood pressure regulation differently.
Risk Factors for Both Types of Hypotension
Orthostatic hypotension and postprandial hypotension share common risk factors such as advanced age, autonomic nervous system dysfunction, and certain cardiovascular conditions including heart failure and diabetes mellitus. Medications like diuretics, beta-blockers, and antihypertensives can exacerbate both types by impairing blood pressure regulation. Dehydration and prolonged immobility further increase susceptibility to episodes of hypotension in affected individuals.
Diagnostic Approaches for Orthostatic and Postprandial Hypotension
Diagnostic approaches for orthostatic hypotension include measuring blood pressure and heart rate changes from supine to standing positions, often using a tilt-table test to evaluate autonomic function. Postprandial hypotension diagnosis involves monitoring blood pressure fluctuations after meal ingestion, typically within the first two hours, to identify significant drops related to digestion. Continuous ambulatory blood pressure monitoring may be employed for both conditions to capture real-world symptoms and guide targeted treatment.
Treatment Options: Managing Drop in Blood Pressure
Treatment options for orthostatic hypotension include increasing fluid and salt intake, wearing compression stockings, and using medications such as fludrocortisone or midodrine to raise blood pressure. Postprandial hypotension management focuses on small, frequent low-carbohydrate meals, avoiding alcohol, and medications like acarbose to slow carbohydrate absorption. Both conditions benefit from lifestyle modifications including gradual posture changes and monitoring blood pressure regularly to prevent dizziness and falls.
Lifestyle Modifications to Prevent Hypotension Episodes
Managing orthostatic hypotension and postprandial hypotension requires targeted lifestyle modifications such as increasing fluid and salt intake to maintain blood volume and consuming smaller, more frequent meals to prevent post-meal blood pressure drops. Incorporating physical counter-maneuvers like leg crossing or calf muscle contractions can improve venous return and reduce dizziness during postural changes. Avoiding alcohol, standing up slowly, and elevating the head of the bed are critical strategies to minimize hypotensive episodes and enhance daily functioning.
Complications and Long-Term Effects of Low Blood Pressure
Orthostatic hypotension can lead to falls, fractures, and cognitive impairment due to repeated cerebral hypoperfusion, increasing morbidity in elderly populations. Postprandial hypotension often exacerbates cardiovascular strain, potentially worsening ischemic heart disease and contributing to syncope-related injuries. Both conditions pose risks of chronic fatigue and reduced quality of life, highlighting the need for careful monitoring and management of low blood pressure complications.
When to Seek Medical Attention for Symptoms
Seek medical attention for orthostatic hypotension if symptoms like dizziness, lightheadedness, or fainting occur upon standing, as these may indicate underlying cardiovascular or neurological conditions. For postprandial hypotension, consult a healthcare provider if experiencing significant drops in blood pressure, dizziness, or falls after meals, which can increase risk of injury and impact quality of life. Persistent or severe symptoms in either condition warrant a thorough evaluation to prevent complications such as syncope or stroke.
Latest Research and Emerging Therapies in Hypotension Management
Recent studies highlight distinct pathophysiological mechanisms between orthostatic hypotension and postprandial hypotension, emphasizing tailored therapeutic approaches. Emerging therapies include novel pharmacological agents such as droxidopa and atomoxetine, demonstrating efficacy in improving autonomic regulation and vascular response. Advances in wearable hemodynamic monitoring devices enable precise diagnosis and personalized management, optimizing patient outcomes in hypotension treatment.
orthostatic hypotension vs postprandial hypotension Infographic
 difterm.com
difterm.com