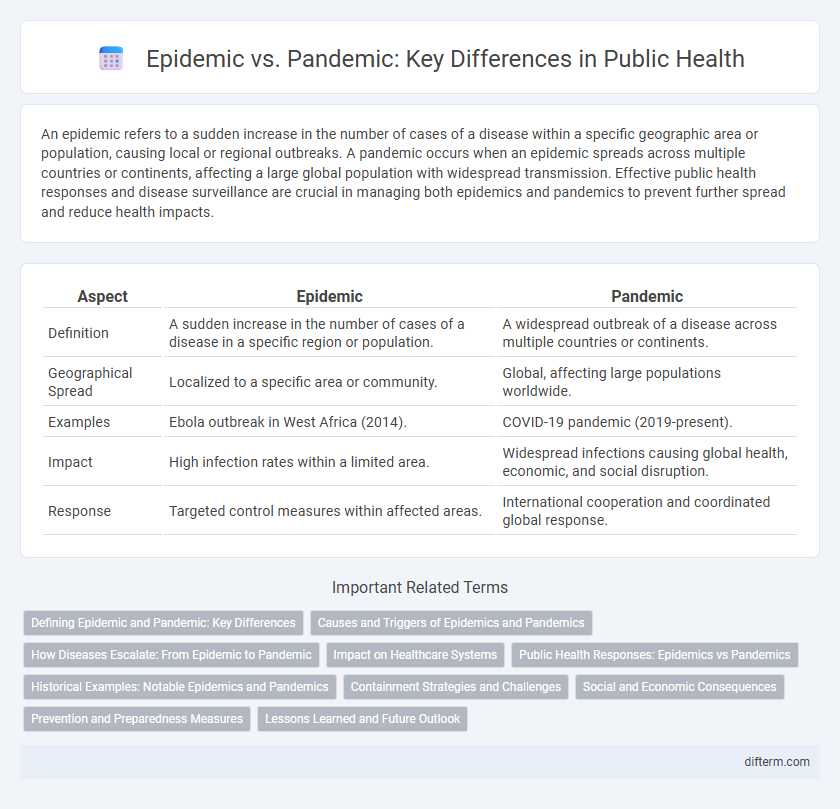
An epidemic refers to a sudden increase in the number of cases of a disease within a specific geographic area or population, causing local or regional outbreaks. A pandemic occurs when an epidemic spreads across multiple countries or continents, affecting a large global population with widespread transmission. Effective public health responses and disease surveillance are crucial in managing both epidemics and pandemics to prevent further spread and reduce health impacts.
Table of Comparison
| Aspect | Epidemic | Pandemic |
|---|---|---|
| Definition | A sudden increase in the number of cases of a disease in a specific region or population. | A widespread outbreak of a disease across multiple countries or continents. |
| Geographical Spread | Localized to a specific area or community. | Global, affecting large populations worldwide. |
| Examples | Ebola outbreak in West Africa (2014). | COVID-19 pandemic (2019-present). |
| Impact | High infection rates within a limited area. | Widespread infections causing global health, economic, and social disruption. |
| Response | Targeted control measures within affected areas. | International cooperation and coordinated global response. |
Defining Epidemic and Pandemic: Key Differences
An epidemic refers to a sudden increase in the number of cases of a disease above what is normally expected in a specific region or population, often localized and limited in scale. A pandemic, by contrast, involves the widespread, global spread of a disease affecting multiple countries or continents, typically with sustained human-to-human transmission. Understanding these key differences is crucial for public health strategies, resource allocation, and managing disease control efforts effectively.
Causes and Triggers of Epidemics and Pandemics
Epidemics and pandemics arise from the spread of infectious agents such as viruses, bacteria, or parasites, often triggered by factors like increased human-to-human contact, zoonotic spillover, or mutations enhancing transmissibility. Environmental changes, urbanization, and global travel accelerate the transmission, facilitating local outbreaks to escalate into widespread pandemics. Public health infrastructure, population immunity, and timely intervention critically influence the trajectory from epidemic emergence to pandemic scale.
How Diseases Escalate: From Epidemic to Pandemic
Epidemics represent the rapid spread of a disease within a localized region or population, often triggered by factors like high contagion rates or environmental changes. When the infection transcends borders and affects multiple countries or continents, a pandemic emerges, driven by global travel, urban density, and pathogen adaptability. Effective public health responses hinge on early detection, containment strategies, and coordinated international collaboration to curb disease escalation from epidemic to pandemic.
Impact on Healthcare Systems
Epidemics strain local healthcare systems by overwhelming hospitals and exhausting medical resources within affected regions, leading to shortages of staff, beds, and essential supplies. Pandemics amplify this impact globally, causing widespread disruptions in healthcare infrastructure, delaying routine medical services, and increasing mortality due to resource allocation challenges. Effective management requires coordinated global responses to distribute medical resources, implement containment strategies, and support frontline healthcare workers to mitigate systemic collapse.
Public Health Responses: Epidemics vs Pandemics
Public health responses to epidemics focus on localized containment strategies, including targeted vaccination campaigns, contact tracing, and quarantine measures within affected communities. Pandemic responses require coordinated international collaboration to implement widespread surveillance, global vaccine distribution, large-scale public education, and robust healthcare capacity building to manage disease spread across multiple countries and continents. Effective risk communication and rapid mobilization of resources are critical to mitigating both epidemic and pandemic impacts on population health.
Historical Examples: Notable Epidemics and Pandemics
The 1918 Influenza pandemic, also known as the Spanish flu, infected nearly one-third of the global population and caused an estimated 50 million deaths, highlighting the devastating impact of pandemics. The Bubonic plague, a notable epidemic in the 14th century, resulted in the Black Death which wiped out approximately 60% of Europe's population. More recent examples include the 2002-2003 SARS epidemic, limited mainly to Asia with around 8,000 cases, and the COVID-19 pandemic that began in 2019, affecting millions worldwide and prompting unprecedented public health responses.
Containment Strategies and Challenges
Epidemic containment strategies often focus on localized interventions such as targeted quarantines, contact tracing, and vaccination campaigns within specific regions, facilitating faster outbreak control. Pandemic containment faces challenges due to widespread transmission across countries, necessitating coordinated global responses, travel restrictions, and mass vaccination efforts, which are complicated by varying healthcare infrastructure and resource availability. Effective management requires real-time data sharing, public compliance with health measures, and addressing misinformation to reduce transmission rates and healthcare system burdens.
Social and Economic Consequences
Epidemics and pandemics both cause significant social disruption, but pandemics tend to amplify economic instability due to their global reach. Social consequences include strained healthcare systems, increased mental health issues, and widespread behavioral changes such as social distancing. Economically, pandemics trigger massive job losses, supply chain disruptions, and long-term impacts on global trade and investment patterns.
Prevention and Preparedness Measures
Epidemic and pandemic prevention and preparedness require robust public health infrastructure, early detection systems, and widespread vaccination campaigns to control disease spread. Community education, quarantine protocols, and international cooperation enhance response effectiveness and reduce transmission rates. Strengthening healthcare capacity, ensuring supply chain continuity, and promoting hygiene practices are critical components in mitigating outbreak impacts.
Lessons Learned and Future Outlook
Epidemics and pandemics reveal critical insights into disease transmission patterns, public health response mechanisms, and healthcare system resilience. Lessons learned emphasize the necessity of early detection, robust surveillance systems, and international cooperation to mitigate widespread impact. Future outlook prioritizes investment in vaccine research, global health infrastructure, and continuous public education to enhance preparedness against emerging infectious diseases.
Epidemic vs Pandemic Infographic
 difterm.com
difterm.com