Polypharmacy increases the risk of adverse drug interactions and medication non-adherence, especially among elderly patients with multiple chronic conditions. Deprescribing aims to reduce medication burden by systematically discontinuing unnecessary or harmful drugs, improving patient safety and quality of life. Careful assessment and collaboration between healthcare providers and patients are crucial to successfully implement deprescribing strategies.
Table of Comparison
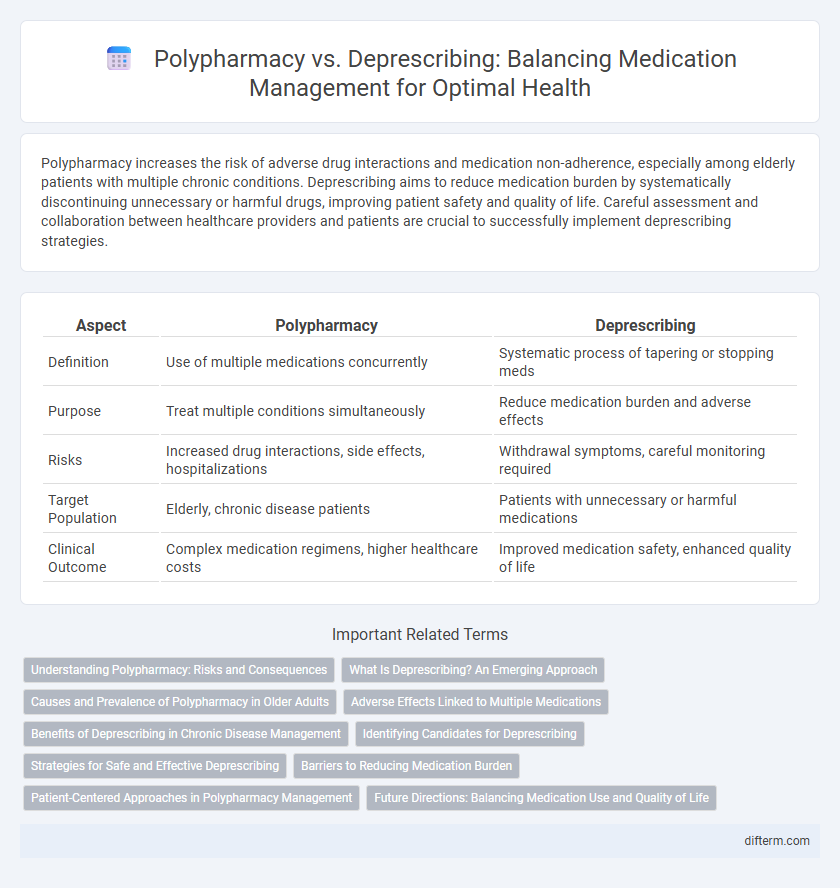
| Aspect | Polypharmacy | Deprescribing |
|---|---|---|
| Definition | Use of multiple medications concurrently | Systematic process of tapering or stopping meds |
| Purpose | Treat multiple conditions simultaneously | Reduce medication burden and adverse effects |
| Risks | Increased drug interactions, side effects, hospitalizations | Withdrawal symptoms, careful monitoring required |
| Target Population | Elderly, chronic disease patients | Patients with unnecessary or harmful medications |
| Clinical Outcome | Complex medication regimens, higher healthcare costs | Improved medication safety, enhanced quality of life |
Understanding Polypharmacy: Risks and Consequences
Polypharmacy, defined as the concurrent use of five or more medications, increases the risk of adverse drug reactions, drug interactions, and medication non-adherence, particularly in older adults. This complex medication regimen often leads to cognitive impairment, falls, hospitalization, and diminished quality of life. Understanding these risks is crucial for healthcare providers to balance therapeutic benefits against potential harms and to consider deprescribing strategies.
What Is Deprescribing? An Emerging Approach
Deprescribing is a patient-centered process that systematically reduces or stops medications that may no longer be necessary or could cause harm, aiming to improve health outcomes and reduce polypharmacy risks. It involves careful review of all prescribed drugs, prioritizing those with potential adverse effects, drug interactions, or diminished efficacy in the elderly or individuals with multiple chronic conditions. Emerging evidence supports deprescribing as an effective strategy to minimize medication burden, prevent adverse drug events, and enhance quality of life in complex patients.
Causes and Prevalence of Polypharmacy in Older Adults
Polypharmacy in older adults commonly arises from multimorbidity, where managing multiple chronic conditions necessitates various medications, increasing the risk of drug interactions and adverse effects. Studies show that nearly 40% of individuals aged 65 and older are prescribed five or more medications, highlighting the high prevalence of polypharmacy in this population. Deprescribing initiatives target reducing unnecessary medications to enhance safety and improve health outcomes among older adults.
Adverse Effects Linked to Multiple Medications
Polypharmacy, defined as the concurrent use of multiple medications, significantly increases the risk of adverse drug reactions, medication non-adherence, and drug-drug interactions, especially in elderly patients with chronic conditions. Deprescribing aims to minimize these negative outcomes by systematically reviewing and reducing unnecessary or harmful medications, thereby improving patient safety and quality of life. Studies show that targeted deprescribing interventions can reduce hospitalization rates related to adverse drug events by optimizing pharmacotherapy regimens in polypharmacy cases.
Benefits of Deprescribing in Chronic Disease Management
Deprescribing in chronic disease management reduces medication burden and minimizes adverse drug reactions, promoting safer pharmacotherapy for patients. This approach enhances medication adherence and improves quality of life by tailoring treatment to individual needs and current health status. Effective deprescribing strategies also lower healthcare costs and prevent drug interactions commonly seen in polypharmacy scenarios.
Identifying Candidates for Deprescribing
Identifying candidates for deprescribing involves evaluating patients with polypharmacy who exhibit high-risk profiles such as advanced age, multiple chronic conditions, or adverse drug reactions. Tools like the Beers Criteria and STOPP/START criteria assist clinicians in recognizing potentially inappropriate medications that may be safely reduced or discontinued. Prioritizing patients with cognitive impairment, frailty, or frequent hospitalizations enhances the effectiveness of deprescribing interventions and improves medication safety.
Strategies for Safe and Effective Deprescribing
Strategies for safe and effective deprescribing involve comprehensive medication reviews, identifying potentially inappropriate medications, and prioritizing those that pose the highest risk for adverse effects. Utilizing patient-centered approaches and interdisciplinary collaboration among healthcare providers enhances adherence and monitoring during the deprescribing process. Implementing evidence-based guidelines and clinical decision support tools further supports optimal medication management and reduces polypharmacy-related complications.
Barriers to Reducing Medication Burden
Barriers to reducing medication burden in polypharmacy include patient resistance due to fear of symptom recurrence, lack of clear clinical guidelines, and limited communication between healthcare providers. Complexity of multiple chronic conditions often complicates deprescribing decisions, leading to clinician uncertainty and inertia. Systemic issues such as time constraints, inadequate reimbursement, and fragmented care coordination further hinder effective medication review and optimization.
Patient-Centered Approaches in Polypharmacy Management
Effective polypharmacy management emphasizes patient-centered approaches that prioritize individual health goals, preferences, and functional status to optimize medication regimens and minimize adverse effects. Deprescribing involves systematic assessment and collaborative decision-making between healthcare providers and patients to safely reduce or discontinue unnecessary medications, enhancing overall quality of life. Integrating comprehensive medication reviews and shared decision-making tools supports personalized interventions that address the complexities of multiple drug use in chronic disease management.
Future Directions: Balancing Medication Use and Quality of Life
Emerging research in polypharmacy emphasizes personalized deprescribing strategies to enhance patient outcomes and reduce adverse drug reactions in aging populations. Integrating advanced decision-support systems and pharmacogenomics can optimize medication regimens tailored to individual health profiles, improving quality of life while minimizing unnecessary drug burden. Future healthcare models prioritize multidisciplinary collaboration to balance effective chronic disease management with deprescribing protocols that safeguard patient safety and functional independence.
Polypharmacy vs Deprescribing Infographic
 difterm.com
difterm.com