Bacteremia refers to the presence of bacteria in the bloodstream without causing symptoms, whereas septicemia is a serious bloodstream infection characterized by systemic inflammatory response and symptoms of sepsis. Early detection and treatment of bacteremia can prevent progression to septicemia, which requires urgent medical intervention to avoid complications such as organ failure. Understanding the differences between these conditions is crucial for effective diagnosis and management in clinical settings.
Table of Comparison
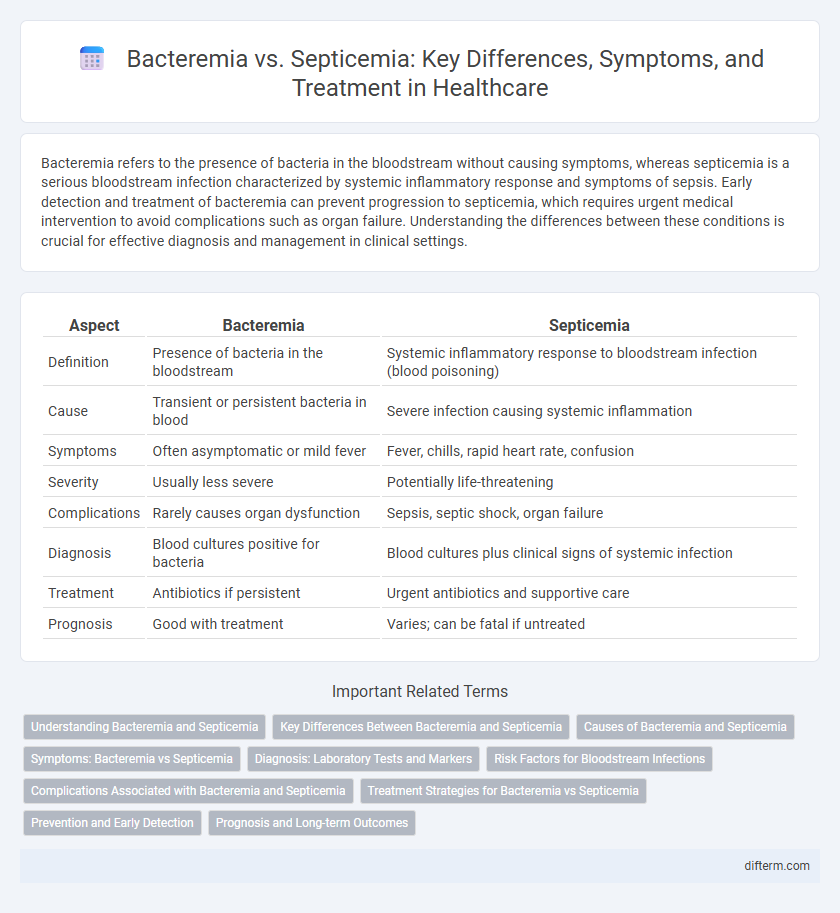
| Aspect | Bacteremia | Septicemia |
|---|---|---|
| Definition | Presence of bacteria in the bloodstream | Systemic inflammatory response to bloodstream infection (blood poisoning) |
| Cause | Transient or persistent bacteria in blood | Severe infection causing systemic inflammation |
| Symptoms | Often asymptomatic or mild fever | Fever, chills, rapid heart rate, confusion |
| Severity | Usually less severe | Potentially life-threatening |
| Complications | Rarely causes organ dysfunction | Sepsis, septic shock, organ failure |
| Diagnosis | Blood cultures positive for bacteria | Blood cultures plus clinical signs of systemic infection |
| Treatment | Antibiotics if persistent | Urgent antibiotics and supportive care |
| Prognosis | Good with treatment | Varies; can be fatal if untreated |
Understanding Bacteremia and Septicemia
Bacteremia refers to the presence of bacteria in the bloodstream, often transient and asymptomatic, whereas septicemia is a serious bloodstream infection causing systemic inflammatory response and potential organ failure. Early detection of bacteremia through blood cultures is crucial to prevent progression to septicemia, which requires immediate antibiotic therapy and supportive care. Understanding the distinction aids in timely diagnosis, improving patient outcomes in critical care settings.
Key Differences Between Bacteremia and Septicemia
Bacteremia is the presence of bacteria in the bloodstream, often transient and asymptomatic, whereas septicemia refers to a systemic inflammatory response caused by bacteria multiplying in the blood, leading to severe infection. Bacteremia may resolve without treatment or progress to septicemia if the immune system fails to contain the bacteria. Septicemia is characterized by symptoms such as fever, chills, rapid heart rate, and can lead to septic shock, requiring prompt medical intervention.
Causes of Bacteremia and Septicemia
Bacteremia occurs when bacteria enter the bloodstream, often caused by infections like pneumonia, urinary tract infections, or dental procedures that introduce bacteria into the circulation. Septicemia, a systemic response to bacteremia, results from the body's overwhelming immune reaction to bacterial toxins, commonly triggered by severe infections such as bloodstream infections, wound infections, or intravascular device contamination. Both conditions require prompt medical attention, as untreated bacteremia can progress to septicemia, leading to sepsis and potentially life-threatening complications.
Symptoms: Bacteremia vs Septicemia
Bacteremia symptoms typically include fever, chills, and rapid heartbeat, often without systemic toxicity signs, while septicemia manifests more severely with high fever, low blood pressure, confusion, and possible organ dysfunction. In septicemia, the body's response to infection causes widespread inflammation leading to symptoms such as rapid breathing, extreme fatigue, and potential septic shock. Early detection of these distinct symptom patterns is critical for effective clinical management and improving patient outcomes.
Diagnosis: Laboratory Tests and Markers
Diagnosis of bacteremia primarily relies on blood cultures, which identify the specific bacteria present in the bloodstream, while septicemia diagnosis involves both blood cultures and clinical assessment of systemic inflammatory response syndrome (SIRS) criteria. Laboratory tests for septicemia include elevated serum lactate levels, procalcitonin, and C-reactive protein, which serve as biomarkers indicating the severity of infection and organ dysfunction. Early detection through these markers and cultures is critical for guiding appropriate antimicrobial treatment and improving patient outcomes.
Risk Factors for Bloodstream Infections
Risk factors for bloodstream infections include immunosuppression, presence of indwelling medical devices, and recent invasive procedures. Bacteremia involves the presence of bacteria in the blood, often linked to localized infections or catheter use, while septicemia denotes a systemic inflammatory response to bacteria in the bloodstream, increasing severity and risk of organ failure. Both conditions are exacerbated by chronic illnesses like diabetes, cancer, and prolonged hospitalization.
Complications Associated with Bacteremia and Septicemia
Bacteremia, the presence of bacteria in the bloodstream, can lead to localized infections and abscess formation if untreated. Septicemia, a severe systemic inflammatory response to blood infection, frequently results in complications such as septic shock, multi-organ failure, and disseminated intravascular coagulation (DIC). Both conditions increase the risk of endocarditis, especially in individuals with pre-existing heart valve abnormalities.
Treatment Strategies for Bacteremia vs Septicemia
Treatment strategies for bacteremia primarily involve targeted antibiotic therapy tailored to the identified pathogen through blood cultures, supported by source control measures such as drainage of abscesses or removal of infected devices. Septicemia requires more aggressive management combining broad-spectrum antibiotics initially, hemodynamic support including fluid resuscitation, vasopressors for septic shock, and intensive monitoring to prevent organ failure. Early intervention and precise antimicrobial stewardship are critical in both conditions to reduce morbidity and mortality rates.
Prevention and Early Detection
Prevention of bacteremia and septicemia relies heavily on maintaining strict hygiene, prompt treatment of infections, and careful management of invasive procedures to reduce bacterial entry into the bloodstream. Early detection involves monitoring symptoms such as fever, chills, rapid breathing, and confusion, combined with rapid blood cultures and inflammatory marker tests like C-reactive protein and procalcitonin. Effective screening and timely antibiotic administration are critical to preventing progression from localized infection to systemic sepsis, thereby reducing morbidity and mortality rates.
Prognosis and Long-term Outcomes
Bacteremia, defined as the presence of bacteria in the bloodstream, generally has a more favorable prognosis when promptly treated with appropriate antibiotics, often resulting in full recovery without significant long-term complications. Septicemia, or sepsis, represents a systemic inflammatory response to bloodstream infection and carries a higher risk of organ dysfunction, prolonged hospitalization, and increased mortality, with survivors frequently experiencing long-term effects such as chronic fatigue, cognitive impairment, and decreased quality of life. Early detection and aggressive management in septicemia are critical to improving survival rates and reducing adverse long-term outcomes.
Bacteremia vs Septicemia Infographic
 difterm.com
difterm.com