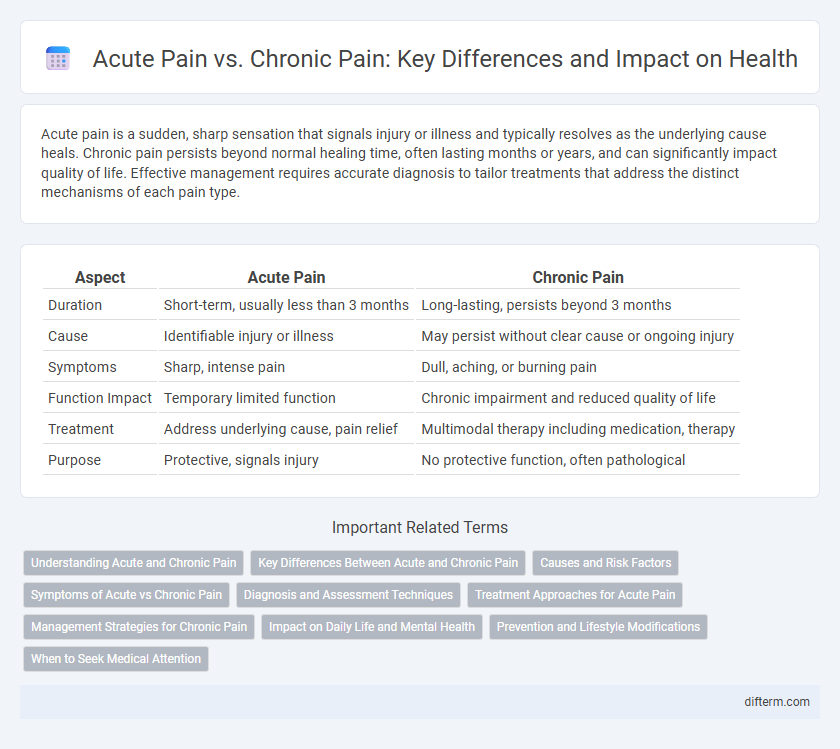
Acute pain is a sudden, sharp sensation that signals injury or illness and typically resolves as the underlying cause heals. Chronic pain persists beyond normal healing time, often lasting months or years, and can significantly impact quality of life. Effective management requires accurate diagnosis to tailor treatments that address the distinct mechanisms of each pain type.
Table of Comparison
| Aspect | Acute Pain | Chronic Pain |
|---|---|---|
| Duration | Short-term, usually less than 3 months | Long-lasting, persists beyond 3 months |
| Cause | Identifiable injury or illness | May persist without clear cause or ongoing injury |
| Symptoms | Sharp, intense pain | Dull, aching, or burning pain |
| Function Impact | Temporary limited function | Chronic impairment and reduced quality of life |
| Treatment | Address underlying cause, pain relief | Multimodal therapy including medication, therapy |
| Purpose | Protective, signals injury | No protective function, often pathological |
Understanding Acute and Chronic Pain
Acute pain serves as a direct and immediate response to injury or tissue damage, typically lasting less than three months and resolving as healing occurs. Chronic pain persists beyond the normal healing period, often exceeding three to six months, and may arise without an identifiable cause, affecting nerve function and quality of life. Differentiating between acute and chronic pain is essential for appropriate diagnosis, treatment planning, and pain management strategies.
Key Differences Between Acute and Chronic Pain
Acute pain is a sudden, sharp sensation usually linked to specific injury or illness, lasting less than three months and serving as a protective warning signal. Chronic pain persists beyond the normal healing time, often exceeding three to six months, and may result from ongoing conditions like arthritis, neuropathy, or fibromyalgia. Unlike acute pain, chronic pain can lead to significant physical and emotional distress, impacting quality of life and requiring comprehensive pain management strategies.
Causes and Risk Factors
Acute pain results from sudden tissue injury such as surgery, trauma, or infection and typically serves as a warning signal for immediate harm. Chronic pain persists beyond normal healing time, often linked to conditions like arthritis, neuropathy, or fibromyalgia, with risk factors including prolonged inflammation, nerve damage, and psychological stress. Understanding these distinct causes and risk factors is essential for targeted pain management and effective treatment strategies.
Symptoms of Acute vs Chronic Pain
Acute pain typically presents as sharp, intense discomfort localized to a specific area and lasts for a short duration, often signaling tissue damage or injury. Chronic pain persists for longer than three months, with symptoms including dull, aching sensations that may be diffuse and can significantly impair daily functions. Unlike acute pain, chronic pain often involves neurological changes, resulting in increased sensitivity and fluctuating intensity.
Diagnosis and Assessment Techniques
Acute pain is typically identified through patient history and physical examination, with diagnostic tools such as imaging and nerve conduction studies used to pinpoint injury or tissue damage. Chronic pain assessment relies heavily on patient-reported outcome measures, psychological evaluation, and functional assessments to understand pain persistence and its impact on quality of life. Quantitative sensory testing and pain diaries are valuable techniques for differentiating between nociceptive, neuropathic, and centralized pain mechanisms.
Treatment Approaches for Acute Pain
Treatment approaches for acute pain primarily focus on addressing the underlying cause, employing analgesics such as NSAIDs and opioids for effective short-term relief. Non-pharmacological interventions like ice application, physical therapy, and nerve blocks play significant roles in reducing inflammation and promoting healing. Timely and appropriate acute pain management is crucial to prevent progression to chronic pain conditions.
Management Strategies for Chronic Pain
Management strategies for chronic pain emphasize a multidisciplinary approach combining pharmacological treatments such as NSAIDs, opioids, and anticonvulsants with non-pharmacological therapies including physical therapy, cognitive-behavioral therapy, and acupuncture. Personalized pain management plans incorporate lifestyle modifications, psychological support, and advanced interventions like nerve blocks or spinal cord stimulation to improve quality of life. Regular assessment and adjustment of treatment based on patient response are essential for effective chronic pain control.
Impact on Daily Life and Mental Health
Acute pain, typically short-term and directly linked to injury or illness, often disrupts daily activities temporarily but usually resolves with healing, minimizing long-term mental health effects. Chronic pain persists beyond normal healing time, severely impairing daily function, reducing quality of life, and increasing the risk of depression, anxiety, and sleep disturbances. Effective pain management and psychological support are critical in mitigating the profound impact of chronic pain on mental well-being and everyday living.
Prevention and Lifestyle Modifications
Effective prevention of acute pain typically involves immediate injury care and avoiding repetitive strain, while chronic pain management emphasizes long-term lifestyle modifications such as regular exercise, stress reduction techniques, and maintaining a healthy weight. Integrating physical therapy, ergonomic adjustments, and balanced nutrition can significantly reduce the risk of persistent pain conditions. Consistent monitoring and adapting lifestyle habits play a crucial role in minimizing the transition from acute to chronic pain, improving overall health outcomes.
When to Seek Medical Attention
Seek medical attention for acute pain if the pain is severe, sudden, or accompanied by symptoms like swelling, redness, or difficulty moving the affected area. Chronic pain warrants professional evaluation when it persists beyond three to six months, disrupts daily activities, or fails to improve with over-the-counter pain medications. Early diagnosis and treatment can prevent complications and improve quality of life.
Acute Pain vs Chronic Pain Infographic
 difterm.com
difterm.com