Myocarditis is inflammation of the heart muscle often caused by viral infections, leading to chest pain, fatigue, and irregular heartbeats. Pericarditis involves inflammation of the pericardium, the protective sac around the heart, causing sharp chest pain that worsens with deep breaths or lying down. Both conditions require medical evaluation but differ in symptoms and treatment approaches, with myocarditis potentially affecting heart function more severely.
Table of Comparison
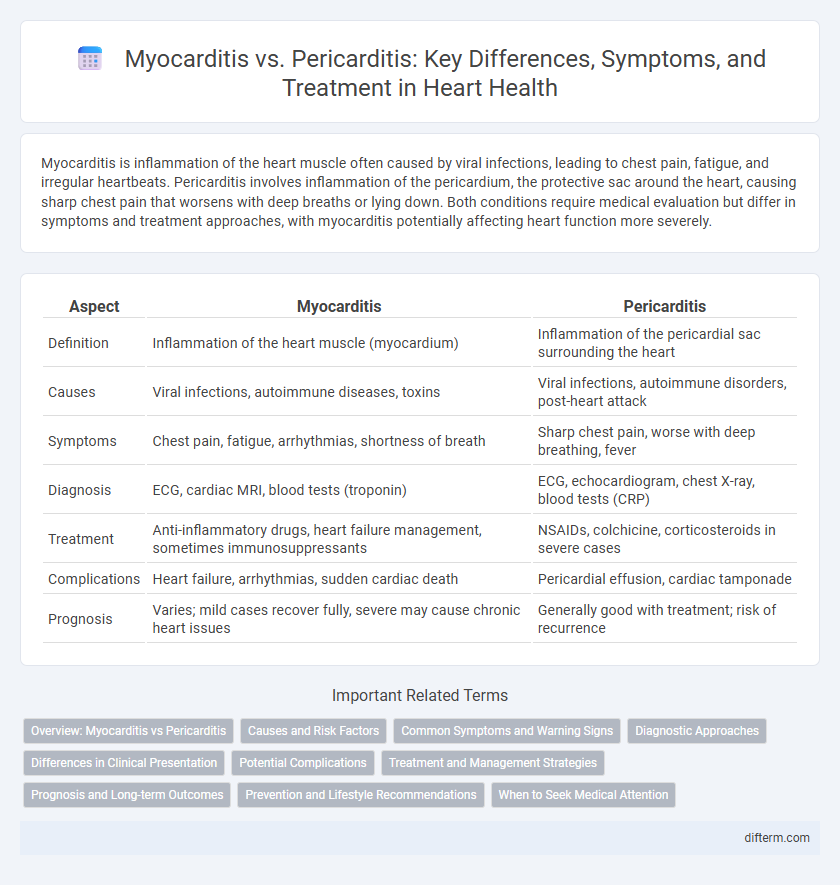
| Aspect | Myocarditis | Pericarditis |
|---|---|---|
| Definition | Inflammation of the heart muscle (myocardium) | Inflammation of the pericardial sac surrounding the heart |
| Causes | Viral infections, autoimmune diseases, toxins | Viral infections, autoimmune disorders, post-heart attack |
| Symptoms | Chest pain, fatigue, arrhythmias, shortness of breath | Sharp chest pain, worse with deep breathing, fever |
| Diagnosis | ECG, cardiac MRI, blood tests (troponin) | ECG, echocardiogram, chest X-ray, blood tests (CRP) |
| Treatment | Anti-inflammatory drugs, heart failure management, sometimes immunosuppressants | NSAIDs, colchicine, corticosteroids in severe cases |
| Complications | Heart failure, arrhythmias, sudden cardiac death | Pericardial effusion, cardiac tamponade |
| Prognosis | Varies; mild cases recover fully, severe may cause chronic heart issues | Generally good with treatment; risk of recurrence |
Overview: Myocarditis vs Pericarditis
Myocarditis is inflammation of the heart muscle, often caused by viral infections, leading to symptoms such as chest pain, fatigue, and arrhythmias, while pericarditis involves inflammation of the pericardium, the protective sac surrounding the heart, typically presenting with sharp chest pain and a pericardial friction rub. Both conditions can result in complications like heart failure or cardiac tamponade but differ in location and clinical presentation. Accurate diagnosis and differentiation rely on imaging techniques such as echocardiography, cardiac MRI, and biomarkers including troponin and inflammatory markers.
Causes and Risk Factors
Myocarditis is commonly caused by viral infections such as Coxsackievirus and COVID-19, while pericarditis frequently results from viral infections, autoimmune diseases, or post-myocardial infarction inflammation. Risk factors for myocarditis include recent viral illness, weakened immune system, and certain medications, whereas pericarditis risk factors encompass recent respiratory infection, systemic inflammatory conditions like lupus, and chest trauma. Both conditions may also be influenced by genetic predisposition and environmental exposures.
Common Symptoms and Warning Signs
Myocarditis and pericarditis both present with chest pain, fatigue, and shortness of breath, yet myocarditis often includes symptoms like rapid heartbeat and fluid retention. Pericarditis typically causes sharp, stabbing chest pain that worsens with deep breaths or lying down. Warning signs for myocarditis involve signs of heart failure and arrhythmias, while pericarditis may lead to pericardial effusion and cardiac tamponade requiring immediate medical attention.
Diagnostic Approaches
Myocarditis diagnosis relies on cardiac MRI, endomyocardial biopsy, and elevated cardiac biomarkers such as troponin, which indicate inflammation and myocyte injury. Pericarditis is primarily diagnosed through clinical evaluation, ECG changes like diffuse ST elevation, echocardiography to detect pericardial effusion, and elevated inflammatory markers such as ESR and CRP. Differentiating these conditions involves integrating imaging findings, biomarker profiles, and clinical presentation to ensure accurate diagnosis and appropriate treatment.
Differences in Clinical Presentation
Myocarditis typically presents with symptoms such as chest pain, fatigue, shortness of breath, and palpitations, often accompanied by signs of heart failure or arrhythmias. Pericarditis primarily manifests as sharp, pleuritic chest pain that worsens with inspiration or lying down, along with pericardial friction rub and sometimes fever. The clinical presentation differences are crucial for diagnosis, as myocarditis involves inflammation of the heart muscle while pericarditis affects the pericardial sac surrounding the heart.
Potential Complications
Myocarditis can lead to severe complications such as heart failure, arrhythmias, and dilated cardiomyopathy due to inflammation of the heart muscle. Pericarditis may result in cardiac tamponade or chronic constrictive pericarditis, impairing heart function through fluid accumulation or thickening of the pericardium. Early diagnosis and treatment are crucial to prevent these life-threatening outcomes.
Treatment and Management Strategies
Treatment for myocarditis primarily involves managing inflammation and supporting heart function, often using medications such as corticosteroids, immunosuppressants, and heart failure drugs like ACE inhibitors or beta-blockers. Pericarditis treatment focuses on reducing inflammation and pain, commonly with nonsteroidal anti-inflammatory drugs (NSAIDs), colchicine, and in severe cases, corticosteroids or pericardiocentesis to remove excess fluid. Both conditions require close monitoring, lifestyle modifications, and addressing underlying causes to prevent complications such as cardiac tamponade in pericarditis or chronic heart failure in myocarditis.
Prognosis and Long-term Outcomes
Myocarditis often results in variable prognosis depending on the severity of inflammation and extent of myocardial damage, with some patients recovering fully while others may develop chronic heart failure or arrhythmias. Pericarditis usually has a more favorable long-term outcome, with most cases resolving completely, though recurrent or constrictive pericarditis can lead to complications requiring ongoing management. Early diagnosis and appropriate treatment significantly improve prognosis in both myocarditis and pericarditis, reducing risks of persistent cardiac dysfunction and mortality.
Prevention and Lifestyle Recommendations
Maintaining a healthy lifestyle with regular exercise, a balanced diet rich in anti-inflammatory foods, and avoiding smoking significantly reduces the risk of both myocarditis and pericarditis. Vaccination against viruses such as influenza and COVID-19 helps prevent infections that can trigger these heart inflammations. Early management of autoimmune diseases and prompt treatment of infections are crucial lifestyle strategies for minimizing complications related to myocarditis and pericarditis.
When to Seek Medical Attention
Seek medical attention immediately if experiencing chest pain, shortness of breath, or palpitations, as these could indicate myocarditis or pericarditis complications. Persistent fever, fainting, or swelling in the legs are critical symptoms requiring urgent evaluation. Early diagnosis through ECG and cardiac MRI improves outcomes and prevents severe cardiac dysfunction.
Myocarditis vs Pericarditis Infographic
 difterm.com
difterm.com