Inflammatory bowel disease (IBD) involves chronic inflammation of the digestive tract, often causing severe symptoms like abdominal pain, diarrhea, and weight loss due to tissue damage. Irritable bowel syndrome (IBS) is a functional disorder characterized by abdominal discomfort and altered bowel habits without underlying inflammation or damage. Accurate diagnosis through medical evaluation is essential to differentiate between IBD and IBS for effective treatment and management.
Table of Comparison
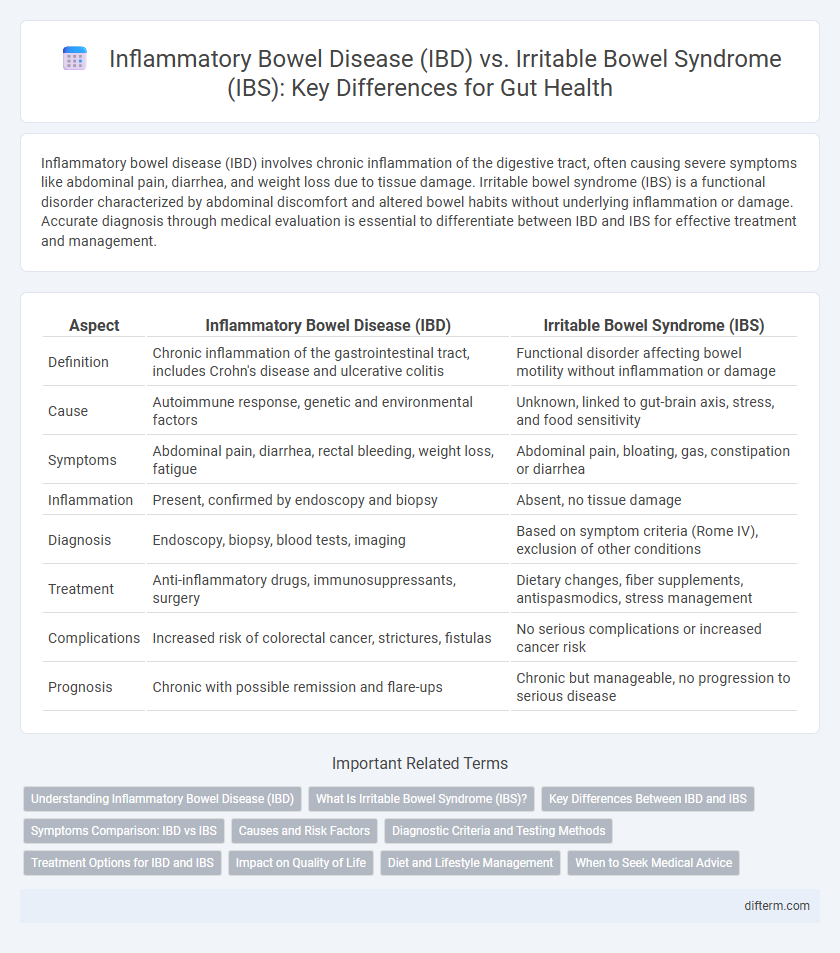
| Aspect | Inflammatory Bowel Disease (IBD) | Irritable Bowel Syndrome (IBS) |
|---|---|---|
| Definition | Chronic inflammation of the gastrointestinal tract, includes Crohn's disease and ulcerative colitis | Functional disorder affecting bowel motility without inflammation or damage |
| Cause | Autoimmune response, genetic and environmental factors | Unknown, linked to gut-brain axis, stress, and food sensitivity |
| Symptoms | Abdominal pain, diarrhea, rectal bleeding, weight loss, fatigue | Abdominal pain, bloating, gas, constipation or diarrhea |
| Inflammation | Present, confirmed by endoscopy and biopsy | Absent, no tissue damage |
| Diagnosis | Endoscopy, biopsy, blood tests, imaging | Based on symptom criteria (Rome IV), exclusion of other conditions |
| Treatment | Anti-inflammatory drugs, immunosuppressants, surgery | Dietary changes, fiber supplements, antispasmodics, stress management |
| Complications | Increased risk of colorectal cancer, strictures, fistulas | No serious complications or increased cancer risk |
| Prognosis | Chronic with possible remission and flare-ups | Chronic but manageable, no progression to serious disease |
Understanding Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease (IBD) encompasses chronic inflammatory conditions such as Crohn's disease and ulcerative colitis, characterized by persistent inflammation of the gastrointestinal tract. Unlike Irritable Bowel Syndrome (IBS), which primarily affects bowel function without causing inflammation or tissue damage, IBD results in significant mucosal injury and complications like strictures and fistulas. Accurate diagnosis through endoscopic evaluation, biopsy, and imaging is essential for targeted treatment to manage inflammation and prevent long-term complications.
What Is Irritable Bowel Syndrome (IBS)?
Irritable Bowel Syndrome (IBS) is a common functional gastrointestinal disorder characterized by chronic abdominal pain, bloating, and altered bowel habits such as diarrhea, constipation, or both. Unlike Inflammatory Bowel Disease (IBD), IBS does not cause inflammation or damage to the intestines and is diagnosed based on symptom criteria and the exclusion of other conditions. Management of IBS involves dietary changes, stress reduction, and medications targeting specific symptoms to improve quality of life.
Key Differences Between IBD and IBS
Inflammatory bowel disease (IBD) involves chronic inflammation and damage to the gastrointestinal tract, including conditions such as Crohn's disease and ulcerative colitis, whereas irritable bowel syndrome (IBS) is a functional disorder characterized by symptoms like abdominal pain and altered bowel habits without visible inflammation. IBD often presents with symptoms such as bloody diarrhea, weight loss, and fatigue, while IBS symptoms typically include bloating, gas, and constipation or diarrhea without systemic signs. Diagnostic methods for IBD include endoscopy and imaging to detect inflammation, whereas IBS is diagnosed through symptom criteria and exclusion of other conditions.
Symptoms Comparison: IBD vs IBS
Inflammatory bowel disease (IBD) symptoms include persistent diarrhea, abdominal pain, rectal bleeding, and weight loss due to chronic inflammation, whereas irritable bowel syndrome (IBS) symptoms primarily involve abdominal pain, bloating, and altered bowel habits without underlying inflammation. IBD often presents with systemic signs like fatigue and fever, while IBS symptoms fluctuate with stress and dietary triggers. Distinguishing IBD from IBS relies on identifying inflammatory markers and endoscopic evidence absent in IBS cases.
Causes and Risk Factors
Inflammatory bowel disease (IBD) is caused by an abnormal immune response leading to chronic inflammation in the gastrointestinal tract, with genetic predisposition and environmental factors like smoking and diet influencing risk. In contrast, irritable bowel syndrome (IBS) stems from dysregulated gut-brain interaction, altered gut motility, and heightened pain sensitivity, often triggered by stress, infections, and food intolerances. While IBD involves structural intestinal damage and immune system malfunction, IBS primarily affects bowel function without causing inflammation or tissue damage.
Diagnostic Criteria and Testing Methods
Inflammatory bowel disease (IBD) diagnosis involves endoscopic evaluation, biopsy, and imaging techniques such as MRI or CT enterography to detect inflammation and tissue damage, alongside laboratory tests for inflammatory markers like C-reactive protein (CRP) and fecal calprotectin. In contrast, irritable bowel syndrome (IBS) diagnosis primarily relies on symptom-based criteria such as the Rome IV criteria, with stool tests used to exclude infections or other organic causes, but lacks specific diagnostic biomarkers or imaging findings. Differentiating IBD from IBS requires comprehensive assessment of clinical presentation, laboratory data, and imaging to identify the presence or absence of intestinal inflammation.
Treatment Options for IBD and IBS
Treatment options for Inflammatory Bowel Disease (IBD) include anti-inflammatory drugs such as aminosalicylates, corticosteroids, immunomodulators, and biologic therapies targeting specific immune pathways. Irritable Bowel Syndrome (IBS) management emphasizes dietary modifications like low FODMAP diet, fiber supplements, antispasmodics, and psychological therapies including cognitive behavioral therapy to alleviate symptoms. Surgical intervention is rarely used for IBS but may be necessary for IBD patients with severe complications such as strictures or fistulas.
Impact on Quality of Life
Inflammatory bowel disease (IBD) significantly impairs quality of life through chronic pain, fatigue, and frequent hospitalizations, often necessitating lifelong treatment and monitoring. Irritable bowel syndrome (IBS) primarily affects quality of life by causing recurrent abdominal discomfort, bowel habit changes, and stress, but it does not cause intestinal damage or increase mortality risk. Both conditions contribute to emotional distress and reduced social functioning, but IBD's impact is generally more severe due to its progressive nature and potential complications.
Diet and Lifestyle Management
Diet and lifestyle management for inflammatory bowel disease (IBD) often requires personalized nutrition plans emphasizing anti-inflammatory foods, adequate hydration, and specific nutrient supplementation to reduce flare-ups and support gut healing. In contrast, irritable bowel syndrome (IBS) management prioritizes a low FODMAP diet to minimize gas and bloating, alongside stress reduction techniques and regular exercise to regulate bowel function. Both conditions benefit from avoiding trigger foods, maintaining a balanced diet, and integrating mindfulness practices to improve overall digestive health.
When to Seek Medical Advice
Persistent symptoms such as severe abdominal pain, unexplained weight loss, blood in the stool, or prolonged diarrhea warrant immediate medical evaluation to differentiate between inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS). Early diagnosis through colonoscopy or imaging tests is vital for managing IBD effectively and preventing complications like bowel obstruction or malnutrition. Patients experiencing sudden symptom worsening or systemic issues like fever should seek urgent care to address potential infections or flare-ups associated with IBD.
Inflammatory bowel disease (IBD) vs Irritable bowel syndrome (IBS) Infographic
 difterm.com
difterm.com